No products in the cart.
No products in the cart.
No products in the cart.
No products in the cart.
Home » Neurological Recovery Blog » Stroke » Understanding Occipital Lobe Stroke: What It Affects & How to Recover
Last updated on October 13, 2022
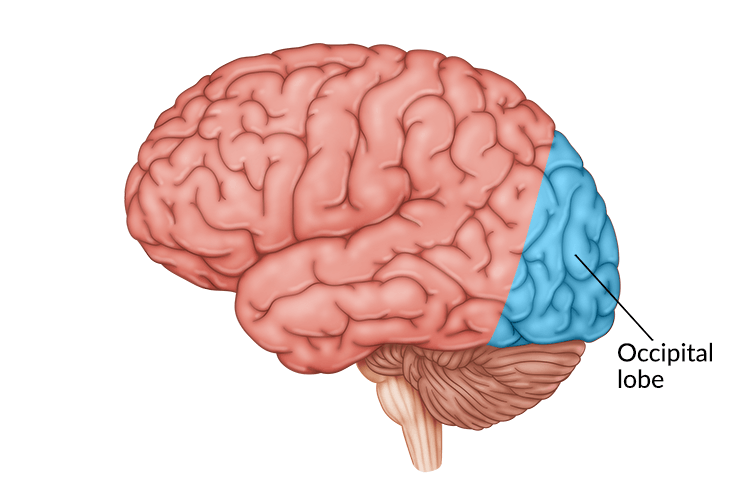
A stroke in the occipital lobe often causes vision problems since this area of the brain processes visual input from the eyes. A stroke can be isolated to the occipital lobe, or it may be more widespread, affecting nearby brain structures such as the cerebellum, brain stem, thalamus, or temporal lobe.
Many occipital lobe stroke survivors sustain hemianopia, or partial blindness. This can be remedied, at least to some degree, through vision restoration therapy. In fact, a new 2021 study focused on survivors of occipital lobe stroke shows that rigorous vision training may help improve hemianopia, even months after the stroke occurred.
This article will discuss everything you should know about occipital lobe stroke, also known as occipital lobe infarct, and the recovery process. Use the links below to jump straight to any section:
A stroke occurs when the supply of blood in the brain becomes disrupted, depriving associated brain tissue of oxygen. There are two types of strokes. Ischemic strokes are most common, making up 87% of all strokes. An ischemic stroke is caused by a blood clot clogging an artery in the brain. When an ischemic stroke occurs in the occipital lobe, it is formally called an occipital infarct.
A hemorrhagic stroke, on the other hand, is caused by a burst or ruptured artery in the brain.
When an artery that supplies blood to the occipital lobe, located in the back of the brain, becomes compromised, an occipital stroke occurs. The occipital lobe is located near the cerebellum, brain stem, temporal lobe, and thalamus. Due to sharing common blood-supplying arteries, a stroke in one of these areas may impact the others.
Common symptoms of a stroke include weakness on one half of the body, facial drooping, and slurred speech. An occipital lobe stroke, however, may not cause these symptoms and instead may cause visual disturbances like blurry vision, hallucinations, or even blindness.
A stroke specifically in the occipital lobe is rare because the arteries in this area have a safety mechanism for blood flow called the “Circle of Willis.” As its name suggests, the Circle of Willis refers to arteries in the brain that are connected in a circle, allowing blood to flow forward or backward to compensate for narrowed or damaged arteries.
Even with this safety mechanism in place, a stroke in the occipital lobe is still possible. When this or any part of the brain becomes deprived of oxygen-rich blood, brain cells begin to die. This can create serious complications, making stroke a medical emergency that requires immediate, swift treatment.
Acute occipital lobe stroke treatment depends on the cause of the stroke. When individuals arrive to the hospital with an ischemic stroke, doctors may use a variety of clot-dissolving drugs, like tPA or aspirin, to restore blood flow in the brain. Hemorrhagic strokes often require more invasive treatment like surgery (often a craniotomy) to stop the bleeding and relieve pressure within the skull.
Correctly diagnosing a stroke is critical for appropriate treatment. Doctors often order a CT or MRI scan to identify the type of stroke and its location so that they can proceed appropriately. For example, while aspirin can be used as emergency stroke treatment due to its blood-thinning effect, it’s only effective for ischemic strokes.
Once a stroke in the occipital lobe has been treated and normal blood flow has been restored in the brain, the road to recovery begins. Survivors will participate in rehabilitation to address any secondary effects that occurred as a result of the stroke.
Many strokes result in a wide array of secondary effects such as motor difficulties or speech difficulties. However, an occipital lobe stroke tends to affect only one specific function: vision.
Because the primary function of the occipital lobe is processing visual input, a stroke in the occipital lobe can result in a variety of vision problems. It is important to note that an occipital lobe stroke does not directly affect the eyes, but rather impedes the brain’s ability to process what the eyes are seeing.
Here are the different types of vision problems that can occur after an occipital lobe stroke:

Each half of the occipital lobe processes visual information from the opposite side of the visual field. Therefore, the right occipital lobe is responsible for processing input from the left visual field, and vice versa. When a stroke affects the occipital lobe only on one side, it can cause blindness on the opposite side of the visual field. For example, a stroke in the left occipital lobe can result in blindness on the right side of the visual field.
Similarly, a stroke in the right occipital lobe can result in blindness on the left side of the visual field, also known as a left visual field cut. This is different from left neglect after stroke, which is an attention problem while hemianopia is a visual problem.
Someone with left neglect may not notice you when approached from the left side because they do not have the cognitive awareness to notice their surroundings on the left half of their body. Someone with a left visual field cut may not notice you when approached from the left because their brain is not processing visual information from that side.

Hemianopia occurs because each half of the occipital lobe processes visual information for the opposite side of the visual field. However, it’s also possible for an occipital lobe stroke to cause a loss of vision in the center of your visual field, a condition known as central vision loss.
When all vision is lost after an occipital lobe stroke, it’s called cortical blindness. This differs from “regular” blindness because the eyes are unaffected, but the visual processing abilities of the brain have been severely compromised.
In rare cases, an occipital lobe stroke can result in vivid hallucinations where survivors see various images like lights, sparks, colorful pinwheels, etc. When visual hallucinations occur while other cognitive functions are preserved, it’s called Charles Bonnet Syndrome.
Prosopagnosia refers to “face blindness” where survivors cannot recognize faces. This may occur when the area responsible for facial recognition, the fusiform gyrus (where the temporal and occipital lobes meet), has been impacted by stroke.
For loved ones, it can be alarming when a survivor does not recognize family members. However, many survivors with prosopagnosia can still recognize voices, so try your best to be patient and understanding and use your voice to remind your loved one of who you are.
Visual agnosia occurs when a survivor cannot identify familiar objects and/or people by sight. This is a subtype of agnosia, a condition that affects the brain’s ability to process what you see, hear, or touch. With visual agnosia, only the ability to process what you see is affected. This can occur after an occipital lobe stroke because this structure of the brain specifically processes vision.
A stroke in the occipital lobe can also cause a condition known as alexia, without a common accompanying condition known as agraphia. Alexia refers to an inability to read or understand written words. Agraphia refers to an inability to communicate through writing.
When an occipital lobe stroke causes alexia without agraphia, it means the survivor cannot read or understand written words but they can still communicate through writing. This is because alexia without agraphia is a visual problem, not a language problem. Reading involves processing visual input while writing involves cognitive language and fine motor skills.
When a stroke only affects the occipital lobe, studies have reported that survivors often have “no significant neurological deficits other than visual-field loss.” If you or someone you know has sustained more than just vision challenges after an occipital lobe stroke, it’s possible that the stroke affected nearby structures in the brain such as the cerebellum, brain stem, temporal lobe, and/or thalamus.
With most secondary effects of an occipital lobe stroke involving vision problems, rehabilitation will revolve around restoring your sight and finding compensatory strategies to make up for visual losses.
Talk to your doctor, who can refer you to a neuro-ophthalmologist or neuro-optometrist. It’s important to see specialists who understand the neurological impact of the stroke on visual processing. A regular optometrist may not be able to help.
After seeing a specialist, some treatment plans may include vision restoration therapy. This rehabilitation method capitalizes on neuroplasticity after stroke, which involves the brain’s ability to heal itself and form new neural networks.
To activate neuroplasticity, vision restoration therapy involves rigorously practicing vision training exercises. Some modalities used include eye movement training (eye exercises), hand-eye coordination exercises, or light therapy. Although research was once very limited, new studies show that intensive visual training may help improve hemianopia (visual field cuts) after an occipital lobe stroke.
Some occupational therapists also receive specialized training to assist individuals with visual challenges. They may be able to educate you in low vision safety strategies, such as placing brightly colored tape on the edge of stairs.
Vision is important for carrying out the activities of daily living, so it’s important to exercise caution and work with trained specialists when your vision has been affected by a stroke.
Depending on their circumstances, some occipital lobe stroke survivors choose to just live with their visual challenges. However, many others have a great desire for improvement. Survivors may wonder if recovery is possible, especially if a significant amount of time has passed since their stroke.
The brain generally heals the most rapidly during the first 3 months after stroke, and rehabilitation during this time often produces faster results than the months or years thereafter. This is also the timeframe where spontaneous recovery is more likely. Spontaneous recovery happens when the brain repairs and salvages the penumbra (the brain tissue surrounding the affected area of the brain) and some functions, such as vision, improve without any intervention. The first three months, therefore, are an excellent time to pursue recovery for any stroke, including occipital lobe strokes.
If a survivor is past the first few months of recovery, they may lose hope for restoring vision after an occipital lobe stroke. Fortunately, the brain is capable of rewiring itself throughout a person’s entire life. Even if it has been many months or years since the event of a stroke, survivors are still encouraged to pursue rehabilitation to maximize their chances of rewiring the brain and improving function.
Every stroke is different and therefore every recovery is different. Some occipital lobe stroke survivors will naturally regain their vision through spontaneous recovery, while others may need to be more intentional about pursuing recovery. Although not everyone regains their vision, there is always hope for recovery through vision restoration therapy at any point.
Overall, there is hope for recovery from occipital lobe stroke. By working closely with your medical team, you can come up with a rehabilitation plan that will help you navigate your new life after stroke.
Not all survivors will benefit from vision restoration therapy, but many will, and it’s important not to give up hope even if you think too much time has passed. Also, be sure to work with an occupational therapist or other specialist to learn how to adapt to any visual changes to ensure your safety throughout the day.
We hope this article helped you understand the effects and recovery process for occipital lobe strokes. For more information, see our comprehensive article on the areas of the brain affected by stroke.
Get our free stroke recovery ebook by signing up below! It contains 15 tips every stroke survivor and caregiver must know. You’ll also receive our weekly Monday newsletter that contains 5 articles on stroke recovery. We will never sell your email address, and we never spam. That we promise.


Do you have these 25 pages of rehab exercises?
Get a free copy of our ebook Full Body Exercises for Stroke Patients. Click here to get instant access.
“My name is Monica Davis but the person who is using the FitMi is my husband, Jerry. I first came across FitMi on Facebook. I pondered it for nearly a year. In that time, he had PT, OT and Speech therapy, as well as vision therapy.
I got a little more serious about ordering the FitMi when that all ended 7 months after his stroke. I wish I hadn’t waited to order it. He enjoys it and it is quite a workout!
He loves it when he levels up and gets WOO HOOs! It is a wonderful product! His stroke has affected his left side. Quick medical attention, therapy and FitMi have helped him tremendously!”
FitMi is like your own personal therapist encouraging you to accomplish the high repetition of exercise needed to improve.
When you beat your high score or unlock a new exercise, FitMi provides a little “woo hoo!” as auditory feedback. It’s oddly satisfying and helps motivate you to keep up the great work.
In Jerry’s photo below, you can see him with the FitMi pucks below his feet for one of the leg exercises:
Many therapists recommend using FitMi at home between outpatient therapy visits and they are amazed by how much faster patients improve when using it.
It’s no surprise why over 14,000 OTs voted for FitMi as “Best of Show” at the annual AOTA conference; and why the #1 rehabilitation hospital in America, Shirley Ryan Ability Lab, uses FitMi with their patients.
This award-winning home therapy device is the perfect way to continue recovery from home. Read more stories and reviews by clicking the button below:
Grab a free rehab exercise ebook!
Sign up to receive a free PDF ebook with recovery exercises for stroke, traumatic brain injury, or spinal cord injury below: