No products in the cart.
No products in the cart.
No products in the cart.
No products in the cart.
Home » Neurological Recovery Blog » Spinal Cord Injury » Pressure Ulcers in Spinal Cord Injury Patients: Causes, Risks, and Management
Last updated on March 16, 2021

Pressure ulcers in spinal cord injury patients are extremely common as a result of impaired motor control and sensation. In fact, the reported annual incidence of pressure ulcers in individuals with SCIs is about 23-30%.
There are many different names for pressure ulcers. Therefore, if you hear the terms pressure sores, bedsores, or decubitus ulcers, know that they all refer to the same condition.
To help you better understand the link between pressure ulcers and spinal cord injuries, this article will explain:
Impaired sensation is the leading reason why individuals with spinal cord injuries develop pressure ulcers. Prior to injury, people typically get the urge to move or shift positions after sitting or lying down for a long time.
Because spinal cord injury disrupts communication between the brain and body, the sensory signals that indicate there is too much prolonged pressure on a specific part of the body are not received by the brain.
As a result, individuals who lose sensation after spinal cord injury tend to no longer feel antsy or uncomfortable when sitting or lying in the same position for an extended period. Consequently, they remain in the same position, accumulating pressure.
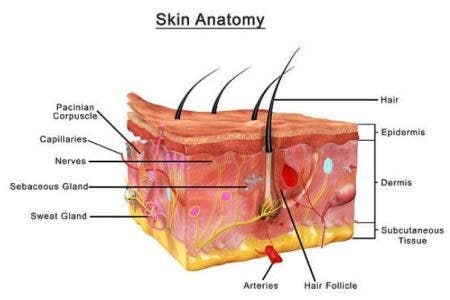
When pressure accumulates for too long, blood flow to that area of the body is disrupted, which deprives the tissues of oxygen. This makes the skin susceptible to breakdown, known as pressure sores.
Additionally, individuals with higher-level spinal cord injuries are generally more likely to develop pressure sores because more areas of their bodies are susceptible to motor impairments and loss of sensation.
Other factors that can contribute to the development of pressure ulcers include:
In the following section, we’ll discuss the stages of pressure ulcer development.
Pressure sores are categorized into 4 stages, with stage 1 being the mildest and stage 4 the most severe.
Below, is a quick overview of each stage:
The earlier pressure ulcers are identified, the easier they are to treat. Likewise, the later pressure ulcers are identified, the greater the risk of additional complications including pain, infections, and in severe cases, death.
While a stage 1 pressure ulcer may only require a few days to heal, a stage 4 pressure ulcer can take anywhere from 3 months to 2 years. Damage to this extent sometimes requires surgical intervention to treat.
Up next, we’ll discuss the best practices for preventing pressure ulcers after spinal cord injury.
The development of pressure ulcers following spinal cord injury is preventable. Therefore, individuals must be made aware of their increased risk and learn how to be proactive about caring for their skin.
Proactive care to prevent the development of pressure ulcers is both cost- and time-effective compared to reactive care for treating an already developed pressure sore.
Below, we’ll go over some actions you can take to prevent getting pressure ulcers in the first place, and to stop the progression of an early stage pressure sore if you do get one.
This is the most important way to prevent pressure ulcers. It’s essential to move the body frequently throughout the day in order to ensure that excess pressure is not being put on any certain part of the body.
Reposition the body every two hours when lying in bed, and do “pressure reliefs” every 30 minutes when sitting up in your wheelchair. Each pressure relief should be held for about 1-3 minutes to be sufficient. Your therapists will be able to show you how to complete pressure reliefs properly.
Individuals with severe weakness or complete paralysis in their upper body will need a caregiver to assist them with repositioning and relieving pressure multiple times a day. For those who can operate a power wheelchair, the tilt and recline functions can be used for pressure relief when sitting up in the chair.
It’s important to have regular skin inspections twice a day to spot pressure ulcers early and prevent them from progressing.
Keep an eye out for changes in skin color, temperature, texture, and moisture levels as they may indicate irritation beneath the surface.
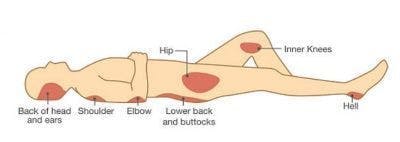
Pressure ulcers are most common in areas where the bones and skin are closely aligned such as the:
Any of these bony prominences where you cannot feel is going to be susceptible to pressure ulcers.
One of the main goals of pressure ulcer management is to prevent the ulcer from growing and compromising the skin around it.
If you notice early signs of a pressure sore, try to remove all pressure on that area as much as possible and apply topical treatments as necessary. If it appears to be a stage 1 ulcer and does not improve within 2 weeks, then follow up with your doctor – do not wait for the wound to get worse! If it is already past the stage 1 phase, report it to your doctor immediately.
Making sure that areas susceptible to pressure ulcers are properly cushioned can help avoid friction.
Consider adding padding to your wheelchair seat as well as the footrests and armrests. Additionally, try to avoid sitting or lying on hard surfaces.
To prevent your ankles or knees from rubbing against each other when lying on your side, try placing a pillow in between the legs.
Making sure the skin is both clean and dry can help reduce the occurrence of pressure ulcers.
This helps ensure that irritants don’t accumulate on the skin. Excess moisture softens and causes swelling of the skin, making it more susceptible to breakdown.
Likewise, it’s important to keep the skin from getting too dry, as it may be more likely to tear.
There are several key recommendations to take care of the skin including:
There are many reasons why poor nutrition can increase the risk of pressure sores.
For one, individuals who are underweight have an increased risk of developing pressure sores due to thinning of the skin and reduced bone and muscle mass.
Our bodies need to consume essential vitamins and minerals to preserve the integrity of the skin. Low body weight and insufficient nutrients are linked to “slow and nonhealing wounds”.
Likewise, being overweight places additional pressure on the skin. Therefore, maintaining a normal weight through a nutrient-dense diet is ideal.
It’s also important to make sure that you’re drinking enough water. When you’re dehydrated, the skin becomes dry and loses elasticity, which increases the risk of pressure ulcers.
Due to impaired motor control and sensation, individuals with spinal cord injuries have an increased risk of developing pressure ulcers.
Pressure ulcers can be costly to treat, force you to take time off work, and can be painful or even life-threatening. This complication of spinal cord injury may be common, but it’s also preventable.
By performing regular skin inspections, cushioning bony areas of the skin, maintaining a healthy weight, and making an effort to reposition the body throughout the day, individuals can minimize their risk of developing pressure sores and improve their quality of life.
We hope this article helped you better understand the risks associated with pressure ulcers following SCI and the most effective ways to prevent them.
Get instant access to our free exercise ebook for SCI survivors. If you liked this post, you’ll LOVE our emails and ebook.
Each exercise features pictures of a licensed therapist to help guide you. You’ll also receive our popular recovery emails with SCI survivor stories and other useful tips — you can opt out anytime.
We will never sell your email address, and we never spam.

Flint Rehab is the leading global provider of gamified neurorehab tools. Check out our bestselling tool by clicking the button below:
Depending on the severity of your spinal cord injury, there may be hope for improved mobility. Consistent at-home therapy is key to making this happen.
That’s why Flint Rehab created FitMi, a motion-sensing, gamified home recovery tool designed for neurological injury like SCI.
Here’s what others have said about it:
“I purchased this wonderful equipment for the use of spasticity for my right hand. Initially I wasn’t sure if it would work because of the various treatments I tried and also many physiotherapists who tried their level best, but didn’t achieve any positive results.
However after trying FitMi, I could feel that slowly and steadily I am improving. It’s really a great device that minutely takes care of each and every muscle of your affected body part. The biggest plus point is, you can use this device anywhere, anytime with precise exercises that you need and also saves your money and time spent on your physiotherapist.“
— Chandrakiran
FitMi works by encouraging you to practice rehab exercises with high repetition. On average, survivors complete hundreds of repetitions per half hour session.
“Massed practice” like this helps stimulate and rewire the nervous system. While you can achieve massed practice with a written sheet of exercises, it can be tough to stick with it consistently — and consistency is key to recovery.
FitMi helps transform rehab exercises into an engaging, interactive experience. The yellow and blue “pucks” track your movement and provide feedback. All of this comes together for a motivating home therapy program.
A survivor named Tom put it perfectly:
“I believe this device will help me concentrate on making the repetitive actions needed to obtain further movement range in my wrist and hand and arm and therefore rating it with five stars. My occupational therapist recommended to give this a try. I have been using FitMi for just a few weeks. I feel more at ease in flexing.”
If you’d like to learn more about FitMi, click the button below:
Do you have this 15 pages PDF of SCI rehab exercises?
Get a free copy of our ebook Rehab Exercises for Spinal Cord Injury Recovery. Click here to get instant access.
Grab a free rehab exercise ebook!
Sign up to receive a free PDF ebook with recovery exercises for stroke, traumatic brain injury, or spinal cord injury below: