Traumatic brain injury medication is administered immediately after an injury to stabilize the individual and prevent a secondary injury. However, a brain injury can result in various secondary effects that may also require medication after initial treatment.
While medication can help relieve many symptoms and secondary effects, such as pain and spasticity, it does not address the root cause of the condition. Therefore, it’s important not to use medication as a substitute for rehabilitation therapy.
This article will discuss the different types of medications used for traumatic brain injury and supplemental ways to promote recovery.
Benefits of Traumatic Brain Injury Medication
Medications play a vital role in both the immediate treatment and long-term management of traumatic brain injury (TBI). While they don’t cure brain injuries, they can significantly reduce complications, ease symptoms, and support the overall recovery process.
Let’s take a look at some of the different ways medication can help following a traumatic brain injury.
How Medication After Traumatic Brain Injury Can Help
Depending on the severity and effects of the injury, medications after a TBI can offer a variety of benefits including:
- Stabilize vital functions: In the emergency phase, medications help control blood pressure, reduce brain swelling, and prevent seizures—crucial for minimizing damage in the early hours after injury. It can also help prevent a secondary injury and lower the risk of complications.
- Reduce pain and discomfort: Over-the-counter or prescription pain relievers can help manage persistent headaches, neck pain, or discomfort that often follows a head injury. Medication may also be used to help manage the various short-term and long-term effects following TBI.
- Manage spasticity and muscle tightness: Muscle relaxants or anti-spasticity drugs can reduce involuntary muscle spasms, stiffness, and twitchy or jerking movements making it easier to move and participate in rehabilitation.
- Support emotional and cognitive function:
Antidepressants, stimulants, or anti-anxiety medications may be used to help regulate mood, improve attention, or reduce irritability and impulsivity in individuals dealing with post-TBI emotional changes. - Prevent secondary complications: Some medications help reduce the risk of blood clots, infections, or other health issues that can develop as a result of immobility or hospitalization.
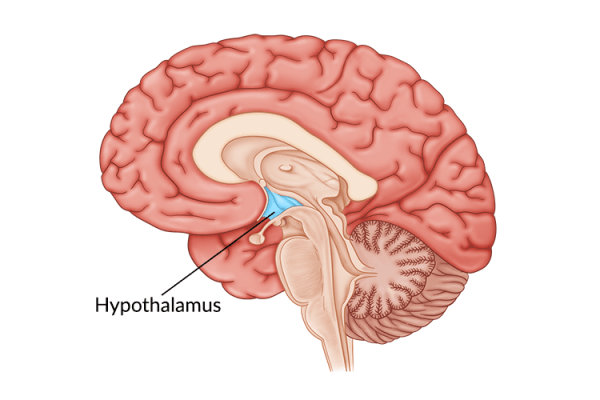
Traumatic Brain Injury Medication and Neuroplasticity
When the brain sustains damage, many of the neural connections used to communicate with other parts of the body may also become damaged or destroyed. Fortunately, the brain can rewire itself and strengthen neural connections through neuroplasticity. To achieve this, individuals must practice high repetition of rehabilitation exercises. The more a task is practiced, the more the brain will reinforce the neural connections for that skill and improve overall function.
While medication can be beneficial, it’s important to understand that it only helps treat the symptoms of certain conditions. Medication for pain or spasticity does not address the root cause of these secondary effects, which is the disruption in communication between the brain and the affected muscles. To address this, survivors must activate neuroplasticity and engage in rehabilitation therapy. This can include a combination of physical, occupational, and speech-language exercises.
It is important to remember that certain medications may have adverse side effects that can interfere with your recovery process. Be sure to speak to your doctor about which medications used for traumatic brain injury are safe and suitable for you. Always follow your doctor’s orders and consult with them before adding or removing any medications from your treatment plan.
What Are the Types of Medications Used for Traumatic Brain Injury?
Medications can address many effects associated with brain injury, from mood disorders to physical pain. However, there are currently no drugs that are FDA-approved to specifically treat the effects of traumatic brain injury. This means the medications listed below are all “off-label.”
The decision to start any medication should be carefully considered with the help of your doctor. They can provide more guidance on which medications are appropriate for you. It should also be noted that many of these medications can have negative side effects and interfere with your recovery process. Be sure to explore alternative options if medication is not appropriate for your condition.
Here are some of the most common types of medications used to treat traumatic brain injury:
1. Pain Medications
One of the most common types of medications administered after a traumatic brain injury is pain medication. Non-opioid analgesics such as acetaminophen, naproxen, and ibuprofen are generally safe for survivors to use. However, certain pain medications, like ibuprofen, should not be taken within the first few weeks post-injury because they can increase the risk of bleeding.
When pain is severe, stronger painkillers may be prescribed. However, strong pain medications, such as opioids and narcotics, work by suppressing brain activity. Therefore, these medications should be taken with caution and for a short period to prevent long-term cognitive damage.
Pain can be exhausting and debilitating, and it can interfere with rehabilitation as well as quality of life. Therefore, pain management is important. Talk to your doctor about which pain medications may be right for you.
2. Psychostimulants
Psychostimulants are medications used to improve cognitive function after a traumatic brain injury. Medications such as Ritalin (also known as methylphenidate) increase frontal lobe activity in individuals who have difficulty with self-regulation and self-control. Although Ritalin is primarily used to treat ADHD, it can also improve alertness after a brain injury. Studies also show that methylphenidate causes a significant improvement in attention and focus in TBI survivors.
Other psychostimulants that doctors may prescribe for traumatic brain injury recovery include Modafinil and Adderall. These can help increase dopamine levels in the brain, boost alertness, and combat extreme cognitive fatigue.
While psychostimulants help improve cognitive function after a brain injury, it’s important for survivors to also engage in cognitive therapy to address the root cause and maximize their chances of recovery.
3. Antidepressants
Depression is one of the most common secondary effects of a brain injury. To be clinically diagnosed with depression, an individual must experience five or more common depression symptoms for at least two weeks. One of the primary symptoms of depression is the feeling of intense sadness or lack of interest in daily activities.
Additional signs of depression after brain injury may include:
- Significant weight loss or weight gain (5% or more in one month)
- Insomnia or excessive sleep
- Motor agitation (making strange movements without meaning to)
- Extreme fatigue
- Feelings of worthlessness
- Decreased concentration or indecisiveness
- Thoughts of death or suicide
To alleviate the symptoms of depression, doctors may prescribe antidepressants. Some of the most common antidepressants prescribed include Fluoxetine hydrochloride (Prozac), Sertraline (Zoloft), Fluvoxamine (Luvox), and Venlafaxine (Effexor).
Antidepressants, especially SSRIs like Prozac, can boost serotonin activity in the brain, which may improve cognitive function. However, some antidepressant medications can cause sedation, which can worsen cognitive dysfunction. Therefore, be sure to consult with your doctor before taking antidepressant medication after a brain injury.
If you feel you are experiencing symptoms of depression or have thoughts of self-harm, get help immediately. Your friends, family, and medical team can help support you and connect you with resources to promote improved mental health and well-being.
4. Antiparkinsonian Agents
Antiparkinsonian agents are another type of medication used for traumatic brain injury. They can help increase dopamine levels in the brain and improve cognitive function. More specifically, studies show that amantadine, an antiparkinsonian agent, may be beneficial for brain injury survivors.
TBI survivors treated with amantadine showed improvements in multiple cognitive functions, including:
- Decreased apathy
- Increased attention, concentration, and arousal
- Improved executive functioning
- Faster processing time
- Reduced agitation, aggression, and anxiety
Another major placebo-controlled study showed that survivors treated with amantadine achieved a significantly faster recovery than those treated with a placebo. Thus, antiparkinsonian agents can be an effective addition to a TBI recovery plan.
5. Antispasmodic Medications
Lastly, antispasmodic medications can help temporarily relieve spasticity or muscle stiffness after traumatic brain injury. The most common types of antispasmodic medication include:
- Tizanidine (Zanaflex): Tizanidine is an oral muscle relaxant typically used for spasticity and other movement disorders caused by a brain injury. This type of medication can help reduce muscle tone for several hours.
- Baclofen: This medication activates GABA receptors, which help produce a relaxing effect on the central nervous system. It can either be taken orally or delivered intrathecally through a surgically implanted pump.
- Botox: This is another common antispasmodic medication that blocks the nerve signals that cause muscles to contract. Botox is injected into specific muscles and generally creates longer-lasting effects (about 3-4 months).
While antispasmodic medications provide temporary relief of spasticity and other muscle conditions, they do not address the root cause, which is the miscommunication between the brain and affected muscles.
The only way to promote long-term spasticity relief is through high repetition of rehab exercises. This will help reinforce demand for those functions in the brain and encourage neuroplasticity. Therefore, it’s important to prioritize rehabilitation exercises while taking medications in the aftermath of a traumatic brain injury.
Medications to Avoid After Traumatic Brain Injury
Not all medications are safe for individuals recovering from a traumatic brain injury. Some drugs may worsen symptoms, interfere with the healing process, or increase the risk of further complications. Knowing which medications to avoid can help protect your recovery and prevent unwanted side effects.
Remember to always follow your doctor’s advice and report any new symptoms or side effects right away.
Common Medications That May Be Harmful After TBI
While your doctor will tailor your treatment plan based on your unique needs, here are some general guidelines on types of medications that are often avoided or used with caution after a brain injury:
- Benzodiazepines (e.g., Valium, Ativan, Xanax): These are typically prescribed for anxiety or sleep, but they can slow brain activity, impair memory, and increase confusion in TBI patients.
- Opioid Painkillers (e.g., Oxycodone, Morphine): While they may be used for severe pain, opioids can lead to drowsiness, reduced cognitive function, and a higher risk of dependency or overdose.
- Antipsychotics with strong sedative effects (e.g., Haloperidol): These may be prescribed for behavioral control but can impair cognitive recovery, especially when used long-term.
- Sleep Aids (e.g., Diphenhydramine, Zolpidem): Over-the-counter or prescription sleep aids may seem harmless, but they can disrupt brain function and worsen fatigue, dizziness, and mood swings.
- Alcohol and recreational drugs: Although not prescribed medications, these substances can interfere with brain healing, increase the risk of seizures, and delay rehabilitation progress.
Remember to always talk to It’s essential to review all medications with your healthcare provider, including over-the-counter drugs and supplements. Everyone’s recovery journey is different, and what may be safe for one person might be dangerous for another. Avoiding potentially harmful medications after a brain injury can support better cognitive function, faster recovery, and fewer complications.
Using Medication After Traumatic Brain Injury
TBI survivors may experience a variety of physical, psychological, and/or cognitive secondary effects. Fortunately, there are many medications used for traumatic brain injuries that can help manage different symptoms and effects of a TBI.
While medication is helpful, it does not address the root cause of the effects, which is the impaired neural connections between the brain and muscles. The best way to treat the root cause and promote recovery is to activate neuroplasticity. This happens when rehabilitation exercises are practiced consistently.
We hope this article helped you understand how medications for traumatic brain injury can be combined with therapy to maximize the chances of making a swift recovery.