In a healthcare world that’s increasingly digital, providers are looking for better ways to support patients between visits. One of the most promising solutions is Remote Therapeutic Monitoring, or RTM. While remote patient monitoring (RPM) focuses on tracking physiological data like blood pressure or glucose levels, RTM goes a step further by monitoring therapy adherence, response to treatment, and patient-reported outcomes, especially in physical therapy, respiratory therapy, and musculoskeletal care.
This guide explains what remote therapeutic monitoring is, how it works, and why it’s gaining attention across clinics and health systems. We’ll also walk through the specific CPT codes that enable providers to bill for RTM services.
Let’s jump in!
Jump to a section:
What Is Remote Therapeutic Monitoring?
Why Is RTM Gaining Popularity?
Who Can Use Remote Therapeutic Monitoring?
What Types of Technology Support RTM?
Remote Therapeutic Monitoring vs Remote Patient Monitoring
Remote Therapeutic Monitoring CPT Codes
Benefits of Remote Therapeutic Monitoring (RTM)
Common Challenges & Considerations for Remote Therapeutic Monitoring
Is RTM Right for Your Practice?
What Is Remote Therapeutic Monitoring (RTM)?
Remote Therapeutic Monitoring (RTM) is a type of digital health service that allows clinicians to monitor how patients are responding to therapy between in-person visits. While it often gets grouped with remote patient monitoring (RPM), RTM serves a different purpose.
Where RPM uses connected devices to collect physiological data like heart rate or oxygen levels, RTM is more focused on therapy adherence and response. That includes data like:
- Pain levels during rehabilitation
- Frequency and quality of home exercise completion
- Mobility or physical function scores
- Self-reported outcomes from patients
RTM gives providers the ability to track these elements through digital platforms, apps, or smart home rehab devices. Most often, it supports patients undergoing musculoskeletal rehabilitation, occupational therapy, physical therapy, or respiratory care.
Why Is RTM Gaining Popularity?
RTM is becoming more widely adopted because it fills a gap in how providers track recovery. For many patients, especially those undergoing rehabilitation, progress doesn’t happen solely in the clinic. Instead, improvement depends on daily exercises, consistent medication use, and symptom tracking, most of which occurs at home.
With RTM, providers gain real-time insights into how patients are doing between visits. This data helps them:
- Identify patients who are struggling before problems escalate
- Adjust treatment plans based on actual patient-reported data
- Increase adherence by keeping patients more accountable
- Improve communication without requiring extra in-person appointments
For patients, RTM can also offer reassurance and motivation. Knowing that their care team is monitoring progress, even remotely, can help keep them on track during the often slow and frustrating recovery process.
Who Can Use Remote Therapeutic Monitoring?
RTM is most commonly used by:
- Physical Therapists (PTs)
- Occupational Therapists (OTs)
- Respiratory Therapists
- Physicians and Qualified Healthcare Professionals (QHPs)
It’s particularly useful in outpatient and home health settings, where long-term recovery and therapy adherence are critical. Providers use RTM tools to monitor a range of conditions, including:
- Post-surgical recovery (e.g., joint replacements)
- Chronic obstructive pulmonary disease (COPD)
- Asthma or other respiratory disorders
- Musculoskeletal conditions (e.g., back pain, arthritis)
- Neurological recovery (e.g., after stroke or brain injury)
What Types of Technology Support RTM?
To implement remote therapeutic monitoring, providers typically use software platforms or smart devices designed for patient engagement and data capture. These may include:
- Mobile apps where patients log daily symptoms or exercise completion
- Wearable motion sensors to measure activity or movement patterns
- Remote rehab tools (like home exercise equipment with feedback features)
The technology must support data collection and secure transmission to providers, as well as allow documentation and tracking that aligns with CMS billing requirements.
Remote Therapeutic Monitoring vs Remote Patient Monitoring
It’s easy to confuse RTM with RPM, but there are some key differences. The following chart takes a look at some of these differences between remote therapeutic monitoring and remote patient monitoring.
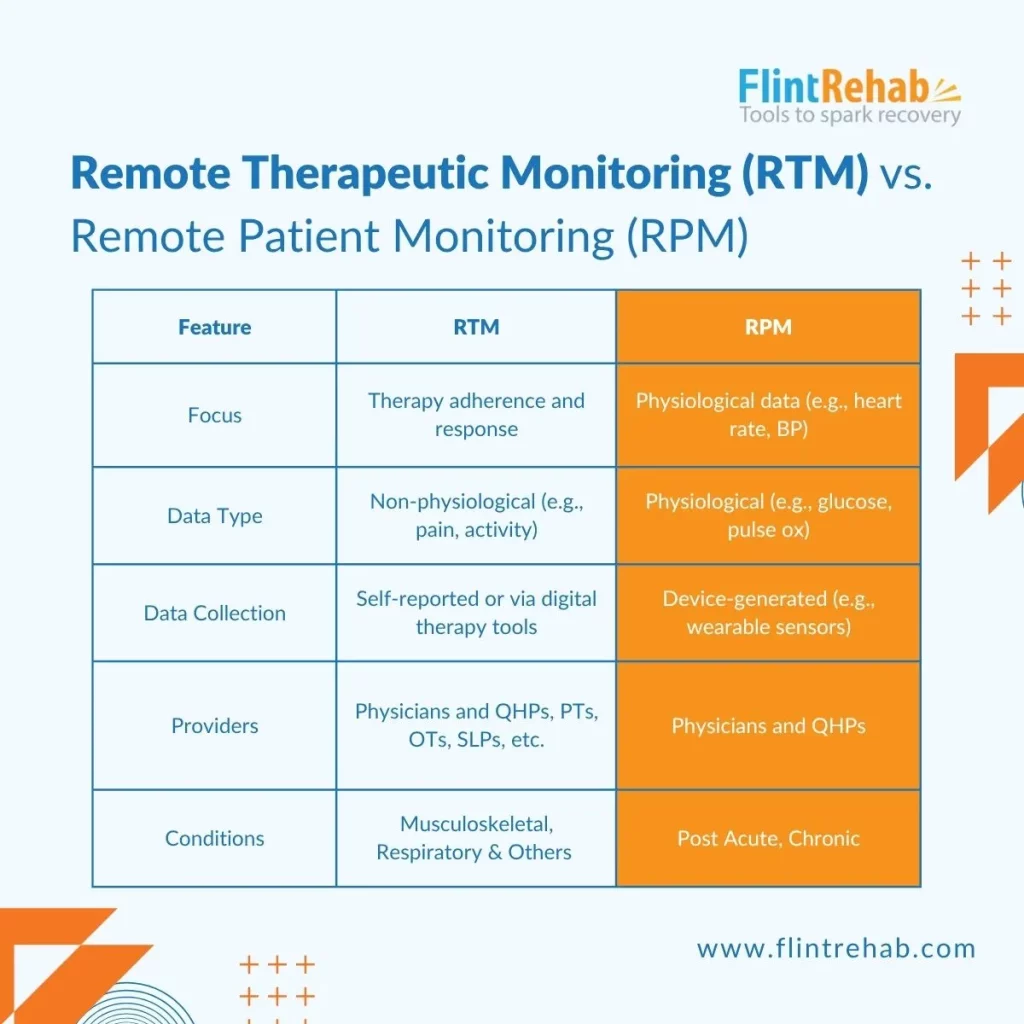
RTM is designed to monitor therapeutic adherence, patient-reported outcomes, and functional progress rather than physiological vitals like heart rate or blood pressure. This makes it more valuable for therapy-focused disciplines such as physical, occupational, and respiratory therapy.
Remote Therapeutic Monitoring CPT Codes
As Remote Therapeutic Monitoring (RTM) continues to grow in physical therapy, occupational therapy, and respiratory care, understanding how to bill for these services is essential. Below is a breakdown of the key RTM CPT codes you need to know—what they cover, how often you can bill them, and what’s required for compliance.
CPT Code 98975: Initial Setup and Patient Education
What it covers:
This code covers the initial setup of the RTM device and educating the patient (or caregiver) on how to use it properly. This includes device installation, app walkthroughs, instructions for logging symptoms or exercises, and setting patient expectations. It’s the foundation for launching a successful RTM episode.
Billing rules:
- Billable once per episode of care
- An episode begins when RTM services start and ends when therapy goals are met
- Requires at least 16 days of data collection during the episode
- Cannot be billed if monitoring falls below the 16-day threshold
CPT Code 98977: Supply of Device for Musculoskeletal Monitoring
What it covers:
This code represents the ongoing supply and use of an RTM device that collects data related to musculoskeletal function. This includes pain levels, range of motion, exercise compliance, and physical activity levels. It applies when the device is used to monitor progress during therapy for conditions like joint pain, arthritis, or post-surgical recovery.
Billing rules:
- Can be billed once every 30 days
- The patient must be actively using the device during this period
- Requires a minimum of 16 days of recorded data per 30-day billing cycle
- Cannot be billed if fewer than 16 days of data are captured
CPT Code 98980: RTM Treatment Management (First 20 Minutes)
What it covers:
This code reimburses providers for the first 20 minutes per calendar month spent managing the patient’s therapy. Activities may include analyzing pain reports, reviewing movement data, adjusting exercise plans, and engaging in direct communication with the patient or caregiver to assess progress or troubleshoot issues.
Billing rules:
- Billable once per calendar month
- Requires at least 20 minutes of documented time
- Must include at least one interactive communication (e.g., phone or video call)
- Not billable if time is under 20 minutes
CPT Code 98981: RTM Treatment Management (Each Additional 20 Minutes)
What it covers:
If you provide more than 20 minutes of RTM treatment management in a month, this code covers each additional 20-minute increment. It includes follow-up conversations, deeper analysis of patient data, or additional clinical decision-making beyond the first 20 minutes.
Billing rules:
- Must be billed in 20-minute increments beyond the initial 20
- Total time must be tracked and documented
- Interactive communication is still required within the calendar month
- Not billable for time less than 20 minutes
What Counts as “Interactive Communication”?
Both 98980 and 98981 require interactive communication to be billable.
According to CMS, this must include:
“A real-time, synchronous, two-way audio interaction that can be enhanced with video or other types of data transmission.”
In plain terms, a phone call or video chat with the patient or caregiver counts. Emails, texts, or portal messages do not satisfy this requirement.
Quick Recap of Billing and Compliance Requirements for RTM Codes
To ensure compliance and maximize billing:
- Confirm at least 16 days of data collection for 98975 and 98977
- Track all provider time spent on RTM management activities
- Ensure interactive communication occurs every month for 98980/98981
- Document patient consent, setup, data reviews, and time logs clearly
One additional thing to note is that for RTM, the service must be ordered by a qualified provider and tied to a specific treatment plan. And while RTM can be billed in conjunction with some evaluation and management services it cannot overlap with RPM billing for the same patient and condition.
Benefits of Remote Therapeutic Monitoring (RTM)
Remote Therapeutic Monitoring (RTM) helps bridge the gap between clinic visits by giving providers real-time visibility into how patients are progressing at home. This data-driven approach offers practical benefits for both healthcare professionals and the individuals they care for.
Why Providers Benefit from RTM
- Real-Time Progress Tracking: Know how patients are doing between visits without relying on memory or infrequent check-ins.
- Smarter Treatment Adjustments: Use real-world data to update therapy plans based on what’s working and what isn’t.
- Bill for Time Already Spent: Get reimbursed for reviewing patient-reported outcomes and remote care management.
- Identify Issues Early: Spot patients who are struggling before it turns into a setback.
- Boost Patient Adherence: Regular feedback encourages better follow-through on home exercises and therapy routines.
Why Patients Benefit from RTM
- Feel More Supported: Patients know their care team is still involved, even when they’re not at the clinic.
- Stay on Track: Reminders and data tracking can improve accountability and motivation.
- Fewer Office Visits: Patients get high-quality care with less travel and disruption to daily life.
- Personalized Recovery: Care is based on their actual progress—not just what gets discussed at appointments.
Common Challenges & Considerations for Remote Therapeutic Monitoring
While RTM offers many benefits, there are a few challenges to consider:
- Technology literacy: Not all patients may be comfortable using digital apps or devices.
- Device costs: Providers need to choose RTM tools that are affordable, reliable, and CMS-compliant.
- Billing complexity: Staying on top of evolving CPT guidance and documentation rules is essential to avoid denials.
- Data security: Patient information must be transmitted and stored according to HIPAA standards.
Training staff and selecting the right platform can go a long way in addressing these hurdles.
Is RTM Right for Your Practice?
If you’re a clinician involved in physical, occupational, or respiratory therapy, remote therapeutic monitoring could be a strong addition to your care model. It enables you to support patients more consistently and provides a billing pathway for the work you already do outside of the clinic.
To get started, consider:
- Identifying common patient groups that would benefit from RTM
- Selecting a user-friendly, HIPAA-compliant platform
- Training your team on documentation and billing procedures
- Educating patients during onboarding so they feel confident using the tools
Final Thoughts on Remote Therapeutic Monitoring
Remote Therapeutic Monitoring is not just a new set of CPT codes—it’s a shift in how we think about therapy and patient engagement. By using technology to bridge the gap between visits, RTM helps clinicians stay connected to patients in meaningful ways. It’s especially useful in musculoskeletal and respiratory care, where daily behavior and therapy adherence directly affect outcomes.
As digital health continues to grow, RTM offers a clear path to smarter, more personalized care—and with the right tools, it’s easier than ever to put it into practice.
Want to learn more about our remote therapeutic monitoring program at Flint Rehab?









