When recovering from a brain injury, it’s natural to focus on the obvious: regaining movement, speech, memory, and independence. But one part of the body that often goes unnoticed in this journey is the gut. More and more research is pointing to a powerful connection between brain health and gut health, and that connection may play a bigger role in brain injury recovery than you think.
In this article, we’ll explore how traumatic brain injuries (TBI) can impact the digestive system, why gut health affects brain function, and what you can do to support both during recovery.
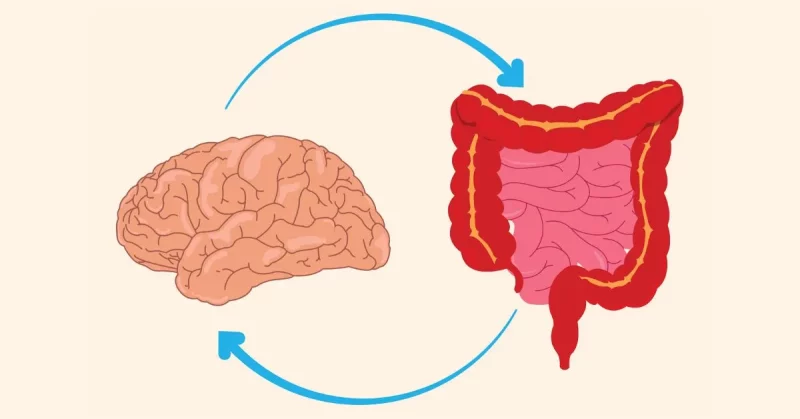
What Is the Gut-Brain Connection?
The gut and brain are in constant communication through a network known as the gut-brain axis. This includes:
- The vagus nerve, a direct line of communication between the gut and the brain
- Neurotransmitters, like serotonin and dopamine, many of which are produced in the gut
- The immune system, which responds to inflammation in both the brain and gut
- The microbiome, the community of bacteria living in the intestines
This two-way communication allows the brain to influence digestion and the gut to affect emotions, cognition, and even behavior.
How Brain Injury Disrupts Gut Health
After a TBI, this finely tuned system can become unbalanced. Here’s how:
1. Damage to the Vagus Nerve
A brain injury may impair vagus nerve function, leading to slower digestion, poor motility, and constipation. This can cause discomfort and reduce appetite, which in turn impacts nutrition—a critical part of recovery.
2. Increased Gut Permeability
Some studies show that brain injuries can make the lining of the gut more porous. This is sometimes called “leaky gut,” and it allows toxins and bacteria to enter the bloodstream, triggering widespread inflammation that can reach the brain.
3. Inflammation and Immune Response
A brain injury typically sparks an inflammatory response, but this inflammation isn’t always contained in the brain. It can spread throughout the body, including the gut, disrupting the balance of healthy bacteria.
4. Medication Side Effects
Medications commonly prescribed after brain injury, including painkillers, antiepileptics, and antibiotics, can interfere with gut bacteria and digestion. These side effects may worsen gastrointestinal symptoms like nausea, bloating, or irregular bowel movements.
The Gut’s Role in Brain Recovery
The gut doesn’t just react to what happens in the brain. It can also influence brain function and recovery. Here’s why supporting your gut may benefit your brain:
Nutrient Absorption
Your gut breaks down and absorbs nutrients essential for brain repair. This includes omega-3 fatty acids, B vitamins, magnesium, and amino acids that support neurotransmitter production.
If your digestive system is compromised, your brain may not receive what it needs to rebuild and recover.
Neurotransmitter Production
Roughly 90% of the body’s serotonin is made in the gut. This chemical helps regulate mood, sleep, and even pain perception. An imbalanced gut microbiome can interfere with neurotransmitter production, potentially worsening anxiety, depression, or insomnia after injury.
Reducing Neuroinflammation
Certain gut bacteria have anti-inflammatory properties. A healthy gut may help lower systemic inflammation, including in the brain. This could make it easier for the brain to heal and form new connections through neuroplasticity.
Symptoms of Gut Issues After Brain Injury
Gut problems can often be subtle, but they may show up as:
- Constipation or diarrhea
- Bloating or abdominal pain
- Acid reflux
- Loss of appetite
- Unexplained fatigue or brain fog
- Nutrient deficiencies
- Mood changes (irritability, depression, anxiety)
If you’re experiencing any of these symptoms, it’s worth discussing with your doctor. These signs could be linked to changes in your gut caused by the brain injury.
Strategies to Support Gut Health After Brain Injury
While there’s no single solution, there are several steps you can take to support your gut during recovery.
1. Focus on Anti-Inflammatory Foods
Eating foods that reduce inflammation may help calm the gut and the brain. Try to include:
- Fatty fish like salmon or sardines
- Leafy greens
- Berries
- Turmeric and ginger
- Olive oil
- Nuts and seeds
Avoid ultra-processed foods, excessive sugar, and fried foods, which can promote inflammation and disrupt gut bacteria.
2. Include Probiotics and Prebiotics
Probiotics are beneficial bacteria found in certain foods and supplements. Prebiotics are fibers that feed these good bacteria.
Good sources include:
- Yogurt with live cultures
- Kefir
- Sauerkraut
- Kimchi
- Garlic
- Onions
- Bananas
- Oats
Talk to your doctor before starting a probiotic supplement, especially if you’re on medications.
3. Stay Hydrated
Dehydration can make constipation worse and affect mental clarity. Drinking enough water helps keep your digestive system moving and supports nutrient absorption.
4. Move When You Can
Physical activity, even gentle stretching or walking, stimulates digestion and helps with regular bowel movements. It can also lower stress, which benefits both the brain and gut.
5. Manage Stress
Stress affects the gut-brain axis significantly. Techniques like mindfulness, deep breathing, meditation, and guided imagery may help regulate this connection and reduce digestive symptoms.
6. Review Medications with Your Doctor
If you notice new or worsening digestive issues, talk to your healthcare provider. Some medications can cause or contribute to gut problems. Adjusting the dose or switching medications may help.
7. Get Your Gut Tested
In some cases, a stool analysis or breath test may be helpful to identify bacterial imbalances, parasites, or poor digestion. Functional medicine practitioners often use these tools to get a clearer picture of what’s going on in the gut.
The Role of the Microbiome in Brain Injury Research
The microbiome is a growing area of research in neuroscience. Animal studies have shown that changing gut bacteria can impact:
- Brain swelling after injury
- Recovery of motor function
- Memory and cognition
- Levels of brain inflammation
Researchers are exploring whether targeting the microbiome with probiotics or diet could improve outcomes after brain trauma. While more human studies are needed, early results are promising and suggest that the gut could play an active role in the healing process.
Can Gut Issues Cause Cognitive Problems After TBI?
It’s possible. The gut influences brain function through:
- Immune signaling. Gut bacteria can trigger immune responses that affect the brain
- Toxin exposure. If the gut becomes too permeable, harmful substances may enter the bloodstream and irritate the brain
- Blood-brain barrier integrity. Some evidence suggests gut bacteria influence the permeability of the blood-brain barrier, which protects the brain from harmful compounds
When these systems are out of balance, people may experience more brain fog, slower processing, irritability, and fatigue.
Brain-Gut Recovery Tips for Caregivers
If you’re helping someone recover from a brain injury, supporting their digestive health might feel like one more thing on a long to-do list. But even small changes can make a difference. Here are a few manageable steps:
- Prepare simple meals with whole ingredients when possible
- Encourage water intake throughout the day
- Track bowel habits to catch signs of constipation early
- Ask the rehab team about safe ways to promote movement
- Create a calm mealtime environment to support digestion
- Keep a symptom journal to share with the healthcare team
When to Talk to a Doctor or Dietitian
Not all digestive symptoms are caused by brain injury, so it’s important to rule out other conditions like:
- IBS (Irritable Bowel Syndrome)
- GERD (acid reflux)
- Food intolerances like lactose or gluten
- Infections or parasites
- Pancreatic insufficiency
Talking with your doctor can help determine the underlying cause of digestive symptoms, which is essential before developing a treatment plan. They may refer you to a registered dietitian who can help create a personalized eating plan, as well as identify potential triggers or deficiencies. They can also guide you through adding supplements if needed.
Final Thoughts
Gut health may not be the first thing that comes to mind after a brain injury, but the connection is strong and worth paying attention to. Supporting your digestive system can ease symptoms, improve mood, and possibly enhance the brain’s ability to recover.
As science continues to learn more about the gut-brain axis, one thing is becoming clear: healing the brain often means healing the body too. And that starts with the gut.