Anosmia refers to the complete loss of smell and can be caused by many neurological conditions, including head injury. Although anosmia affects around 20% of individuals following traumatic brain injury, this problem is commonly overlooked and is often discounted by health professionals as being a minor concern or annoyance. Conversely, post-traumatic anosmia can lead to decreased enjoyment of daily activities and have a major impact on a person’s quality of life.
However, there is hope for recovery as well as several techniques to compensate for anosmia. In this article we will review the different causes of anosmia after head trauma as well as treatments to help you cope with this condition.
Table of contents:
Causes of Post-Traumatic Anosmia
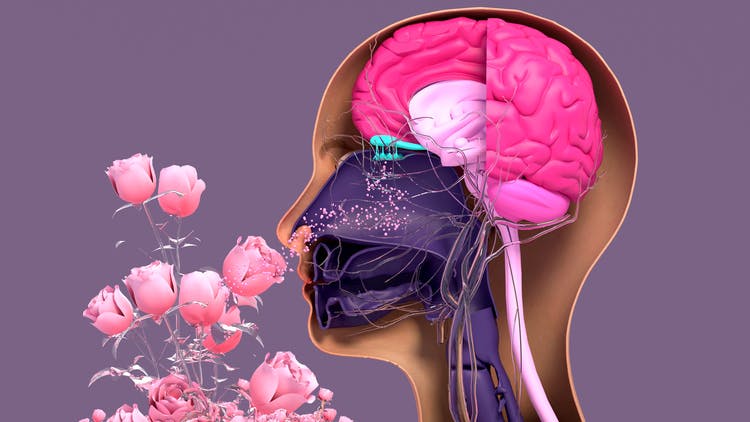
Post-traumatic anosmia, also known as smell blindness, is caused by damage to the nerves or parts of the brain that control your sense of smell. The three main areas we will discuss, among others, work together to detect and process olfactory input, or input for the sensation of smell. Disruption or injury to these structures can prevent olfactory processing, resulting in anosmia. These structures include:
- The olfactory cortex. This cortex is a grouping of multiple areas of the brain that receive input from the olfactory bulb. This information is then sent to the orbitofrontal cortex, located above and behind the eyes, as well as the hypothalamus and brainstem.
- The olfactory nerve fibers. Also called the olfactory bulbs, these groups of nerve fibers are located on the underside of the brain, directly above the nasal cavity. These nerve fibers relay smell sensation to the brain via the olfactory tract.
- The insula. This structure lies deep within the lateral sulcus of the brain, separating several of the major lobes. The insula plays a role in detecting smells that are potent or unpleasant and also impacts perception of taste.
Anosmia after head injury is often due to injury to the olfactory cortex, the area of the brain responsible for processing smell. Contusions or hemorrhage in this area of the brain can cause compression or tissue damage, resulting in inhibited processing of olfactory input and, therefore, anosmia.
Shearing or severing of the olfactory nerve fibers often results from a type of head injury called a coup-contrecoup injury. These injuries are commonly caused by falls or motor vehicle accidents. Depending on the severity of the injury, smell may be partially diminished or absent all together, resulting in anosmia.
Damage to the insula can impair odor processing, causing smells that were previously pleasant to be interpreted as unpleasant or harsh. This can be referred to as dysosmia or phantosmia, which we will discuss in the next section.
Additionally, another potential cause of anosmia after head injury is disruption of the sinonasal tract. Fracture of the nasal bones forming this tract can block the passageway or lead to scarring, preventing reception of olfactory stimulation. Furthermore, if the skull’s cribriform plate (the piece of bone directly behind the nose) is shattered, this could sever the olfactory nerves.
Other Disorders of Smell After Brain Injury
In addition to anosmia, head injury can lead to other smell disorders that don’t result in the complete loss of smell. Although individuals with these conditions may not lose their smell entirely, this can still be frustrating or irritating and can dramatically affect daily activities.
Disorders of smell besides anosmia include:
- Hyposmia: Partial loss of smell
- Hyperosmia: Enhanced sense of smell
- Phantosmia: False or imaginary smells
- Dysosmia: Distortion of smells
When a person suffers from dysosmia, for example, sour milk might smell fresh to them, or fresh flowers might smell rotten and dead. Alternatively, if a person is affected by phantosmia they may detect smells that aren’t really there. These smells can be pleasant or unpleasant and generally come and go, although there are some cases where the smell is persistent.
Complications of Anosmia After Head Trauma
Anosmia can have a considerable impact on daily life and affect many activities in ways most people do not realize. Following head trauma, anosmia can lead to a variety of complications such as:
- Loss of taste. Taste and smell are intimately connected and, unfortunately, this means anosmia can impair your sense of taste as well. Most people with anosmia can only taste very spicy or very salty foods.
- Weight loss. Lack of smell and taste can cause a decrease in appetite and lack of enjoyment at mealtimes. This can lead to rapid, unhealthy weight loss.
- Food poisoning. Altered or absent smell can result in the inability to smell spoiled food, increasing risk of developing food poisoning.
- Memory impairments. The olfactory bulbs connect to the amygdala, the part of the brain in charge of emotions and personal memories. As a result, anosmia can negatively impact the brain’s capacity to code new memories.
- Fire hazards. Anosmia can impair a person’s ability to detect smoke and other harmful chemicals. This increases a person’s risk of injury from situations such as a fire or gas leak.
- Depression. Losing the ability to taste and smell can cause a lack of enjoyment from normal daily activities as well as decreased social involvement. These factors can lead to feelings of hopelessness and depression.
Diagnosing Anosmia After Head Injury
Anosmia is often overlooked after head injury because initial treatment is generally focused on the most life-threatening or serious injuries. In addition, some patients do not recognize their altered or absent smell until weeks later when the initial stage of recovery has passed and they are able to focus on other factors.
As we discussed earlier in the article, around 20% of patients with head injury experience anosmia or other olfactory involvement. It is important to recognize and diagnose this condition as early as possible to help avoid subsequent complications and maximize recovery.
The most widely used diagnostic test for anosmia is the University of Pennsylvania Smell Identification Test (UPSIT). This test evaluates a person’s ability to distinguish smells by using 40 scratch-and-sniff cards. The test is scored in the following way:
- Normosmia: normal smell function
- Mild Microsmia: mild smell impairment
- Moderate Microsmia: moderate smell impairment
- Severe Microsmia: severe smell impairment
- Anosmia: no smell function
This test is able to recognize anosmia after head trauma and allows individuals to get the help they need to recover or cope with this condition. Now that we’ve reviewed the different types and complications of anosmia, let’s discuss treatments and techniques for compensation.
Treating Post-Traumatic Anosmia
Research suggests that around 30% of individuals with anosmia after head trauma regain their sense of smell naturally. This recovery generally occurs between 6 and 12 months following the injury. Additionally, individuals with less severe impairment have a greater chance of recovering olfactory function.
For people with a distorted sense of smell, some medications such as Gabapentin can help. Unfortunately, at this time there are very few treatments available to reverse anosmia after head trauma. However, a newer therapy called olfactory training seems to hold promise.
Olfactory training involves inhaling strong scents such as rose, eucalyptus, and lemon. This stimulates the olfactory nerves in the nose in the hopes of retraining the brain to detect smells. This treatment has been shown to increase olfactory sensitivity in 30 percent of people affected by anosmia after head trauma.
Although resolution of anosmia generally occurs in the 6 to 12 month timeframe, there have been several known cases where spontaneous recovery has occurred years after the injury. There is also some evidence to suggest that the use of zinc or a corticosteroid can promote recovery of smell, although this evidence is still limited.
Coping with Loss of Smell After Head Injury
If your anosmia does not improve or resolve, you will need to learn techniques to cope with loss of smell and taste. Although this condition can be frustrating for survivors, there are many ways to help lessen the impact of anosmia after head trauma. Finding coping mechanisms that fit within your lifestyle can help keep you safe and enhance your quality of life.
Here are a few ideas to help you cope with anosmia after head trauma:
- Use seeds and nuts to add texture. While these won’t restore your sense of taste or smell, adding different textures can help your meals seem less bland. For example, foods such as nuts, seeds, or breadcrumbs can add crunch to meals. This might increase your appetite and enjoyment of mealtimes, potentially helping you gain back lost weight.
- Throw out expired food. For individuals with anosmia, it’s important to keep track of expiration dates and visually inspect food before eating. This can help prevent stomach upset or food poisoning.
- Install smoke and gas detectors. This is crucial, especially if you live alone. These devices can warn you of a fire or gas leak since anosmia can prevent you from recognizing these dangers yourself.
- Use caution when working with chemicals or household cleaners. Individuals with anosmia may not recognize harsh chemical smells created by household cleaners or other substances, such as paint. When using any of these products, make sure the house is well ventilated and consider using a mask to avoid inhalation of fumes.
- Try ice cube stimulation. If anosmia impaired your sense of taste, ice cube stimulation might help. Some patients report that sucking on an ice cube for one minute before a meal helped improve their sense of taste. In particular, it restored their ability to taste sweet foods. While more studies are needed to understand why this happens, it might be a technique worth trying.
Lastly, it is important to lean on your friends and family for support as you cope with anosmia and navigate life after head injury. If you can, find a support group to connect with other survivors and talk with your provider about other possible resources.
Understanding Anosmia After Head Trauma
Anosmia is a condition characterized by the loss of smell, often resulting from damage to the olfactory cortex or olfactory nerves caused by head trauma. Besides impairing smell, anosmia can cause a person to lose their sense of taste and can lead to decreased enjoyment of daily activities as well as other complications.
While there are few available treatments for anosmia after head injury, olfactory training may be beneficial. Talk to your doctor for more information on treating anosmia. New therapies are on the rise, and your doctor might know of other potential treatments to help with this condition.
Some cases of anosmia resolve automatically with time. If that does not occur, however, there are many coping strategies that can help make life without smell safer and more enjoyable. We hope this article helped explain anosmia after head injury as well as possible treatments and compensations to maximize quality of life.