Tactile agnosia is a rare neurological condition that affects a person’s ability to recognize objects by touch alone. While vision or hearing may remain intact, the sense of touch becomes unreliable for identifying everyday items. This can be confusing and frustrating, especially when the individual can physically feel the object but cannot say what it is.
In this article, we’ll explore what tactile agnosia is, what causes it, how it differs from other sensory conditions, and what treatment options are available.
Jump to a section:
How Tactile Agnosia Differs from Other Sensory Disorders
How Tactile Agnosia Is Diagnosed
Challenges and Coping Strategies for Tactile Agnosia
Best Treatment Options for Tactile Agnosia
Long Term Outlook for Patients With Tactile Agnosia
Tactile Agnosia Frequently Asked Questions
What Is Tactile Agnosia?
Tactile agnosia is a type of agnosia that affects somatosensory processing, specifically the ability to identify objects through touch.
This condition may include:
- Ahylognosia: the inability to recognize the properties of an object through touch, such as the weight, density, or texture
- Amorphognosia: inability to identify the shape or size of an object through touch
Some people with this condition may be able to describe the shape, texture, and/or size of an object, but still fail to recognize what it is without using vision or sound.
For example, someone might hold a key in their hand and feel its ridges and metal texture, yet still be unable to identify it as a key unless they look at it. Alternatively, they may be able to hold a ping pong ball and recognize it is circle shaped, but be unable to identify that it is made of plastic or light weight.
How Does Tactile Agnosia Happen?
The brain typically uses sensory input from the skin, muscles, and joints to build a mental image of what’s being touched. For people with tactile agnosia, the sensory input reaches the brain, but the interpretation process breaks down.
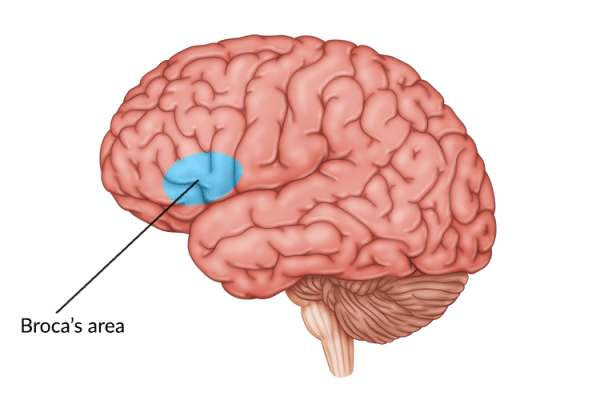
This often happens due to damage in the parietal lobe, particularly the somatosensory cortex or its connections to other brain areas responsible for recognition and memory.
Identifying Tactile Agnosia: Looking at the Key Characteristics of Tactile Agnosia
Identifying tactile agnosia involves understanding the key characteristics of the sensory condition. In other words, understanding what it affects and what it doesn’t.
Here is a short breakdown of the common preserved and impaired abilities for individuals with tactile agnosia.
Preserved Abilities:
- Touch perception is intact: People can feel pressure, temperature, pain, and texture.
- Motor function remains normal: They can grasp, manipulate, and explore objects.
- Vision and language skills are not always affected: Many can identify objects by sight or describe them verbally when prompted.
Impaired Abilities:
- Object recognition by touch is lost: Even familiar items may not be recognized without looking.
- Tactile-based naming fails: The person may struggle to name or explain the object being held.
These traits make tactile agnosia distinct from other sensory deficits such as numbness or blindness. The issue is not with sensation itself but rather with the brain’s ability to interpret the tactile information.
Causes of Tactile Agnosia
Tactile agnosia typically results from damage to specific areas of the brain. This damage can be caused by several conditions or events:
1. Stroke
A stroke affecting the parietal lobe, especially the supramarginal or angular gyrus, can disrupt the integration of touch and object recognition. This is one of the more common causes in older adults.
2. Traumatic Brain Injury (TBI)
Head injuries can impact multiple regions of the brain, including those responsible for tactile perception. Depending on the severity and location of the injury, tactile agnosia may appear alongside other forms of agnosia or cognitive impairments.
3. Brain Tumors
A tumor pressing on the parietal lobe or its pathways can interfere with somatosensory processing and lead to tactile agnosia, either gradually or suddenly depending on the tumor’s growth rate.
4. Neurodegenerative Diseases
In rare cases, conditions like Alzheimer’s or corticobasal degeneration may impair tactile recognition as part of broader sensory and cognitive decline.
5. Post-Surgical Complications
Brain surgeries, especially those involving tumor removal or seizure control in the parietal lobe, can sometimes lead to sensory interpretation problems including tactile agnosia.
How Tactile Agnosia Differs from Other Sensory Disorders
Tactile agnosia can be confused with other sensory disorders. Understanding the difference helps in making a proper diagnosis.
Tactile Agnosia vs. Astereognosis
Astereognosis is often used interchangeably with tactile agnosia, but they can differ slightly. While tactile agnosia refers to the failure of object recognition through touch alone, astereognosis may also involve a broader impairment of tactile exploration and tactile perception deficits, especially if motor or sensory loss is present.
Tactile Agnosia vs. Sensory Deficits
Conditions like peripheral neuropathy can cause numbness or reduced touch sensation. These differ from tactile agnosia, where sensation is intact but interpretation is impaired.
Tactile Agnosia vs. Apraxia
Apraxia involves difficulty performing learned movements or tasks, often due to motor planning issues. In contrast, tactile agnosia is not a problem of movement but of sensory interpretation.
How Tactile Agnosia Is Diagnosed
Diagnosis typically involves a combination of neurological exams, imaging, and tactile recognition tests.
- Clinical Assessment: A neurologist or occupational therapist may perform a series of tasks that involve blindfolding the patient and placing familiar objects in their hands. If the patient can describe the object but not name it, tactile agnosia may be suspected.
- Neuroimaging: MRI or CT scans can reveal damage or abnormalities in the parietal lobe or related areas. This helps confirm the cause and guides treatment planning.
- Additional Testing: To rule out other issues, sensory testing for temperature, pressure, and pain may be conducted. Cognitive and motor skills are also assessed to distinguish tactile agnosia from other conditions.
Challenges and Coping Strategies for Tactile Agnosia
Though rare, tactile agnosia can significantly impact daily life. Recognizing objects without sight is something most people do automatically, so losing this ability often leads to frustration or a sense of dependence.
Challenges of Living With Tactile Agnosia
- Self-care tasks: Brushing hair, using utensils, or buttoning a shirt may become difficult without looking.
- Safety concerns: Identifying hot surfaces or sharp objects by touch becomes unreliable.
- Emotional toll: Frustration and embarrassment may result from repeated failures to recognize everyday items.
Coping Strategies for Tactile Agnosia
- Use of vision: Relying more on visual cues can help compensate for the loss of tactile recognition.
- Labeling items: Adding visual labels to common objects can make them easier to identify when needed.
- Routine and repetition: Creating predictable routines reduces the number of items one needs to identify by touch.
Tactile Agnosia: Best Treatment Options and Strategies
There is no single treatment that completely restores the ability to recognize objects by touch, but targeted rehabilitation strategies can make a meaningful difference. The goal is to maximize independence and function by retraining the brain, adapting daily routines, and providing support tools that reduce frustration and confusion.
Below are the primary treatment options available:
1. Occupational Therapy
Occupational therapy is often the foundation of treatment for tactile agnosia. Therapists focus on helping individuals adapt their environment and develop workarounds that allow them to complete everyday tasks more easily.
Goals of occupational therapy for tactile agnosia include:
- Teaching clients how to perform tasks using vision instead of touch
- Structuring daily routines to minimize reliance on tactile recognition
- Encouraging the use of labeling systems or color-coded containers
- Developing confidence and problem-solving strategies in daily life
For example, a person who struggles to identify grooming tools by feel might learn to organize items by shape and size, or keep them in specific trays with visual cues to help distinguish them.
Therapists may also work with caregivers to make home environments more navigable. This can include decluttering, using consistent item placement, and introducing tactile-friendly alternatives such as textured grips or distinct shapes for commonly used items.
2. Sensory Re-education
Sensory re-education helps the brain rebuild or strengthen the pathways involved in recognizing objects through touch. It involves structured activities that gradually increase in complexity, allowing the brain to relearn how to connect sensation with meaning.
Common sensory re-education exercises include:
- Object matching games: Patients are given pairs of objects and asked to match them using only touch. This helps re-establish the link between tactile input and object features.
- Texture identification tasks: Using materials like sandpaper, velvet, rubber, or silk, patients are encouraged to distinguish textures while blindfolded.
- Progressive tactile challenges: Tasks become more complex over time, such as identifying coins, buttons, or tools from a group using only hands.
Sessions are typically led by an occupational therapist or neurorehabilitation specialist and may be incorporated into a larger therapy plan. The key is repetition and increasing difficulty to encourage brain adaptation.
3. Neuroplasticity-Based Exercises
The brain has a remarkable ability to rewire itself through neuroplasticity, especially when it comes to relearning lost skills after injury. With consistent and targeted stimulation, new neural connections can form, allowing the brain to adapt to deficits like tactile agnosia.
Examples of neuroplasticity-based strategies for tactile agnosia:
- Repetitive object handling: Handling a wide variety of objects with different textures, weights, and shapes to stimulate touch receptors and memory recall
- Multi-sensory training: Combining touch with other senses, such as vision or sound, to help reinforce object identity (e.g., holding a bell while listening to its ring)
- Mirror therapy: In cases where tactile agnosia affects only one hand, mirror therapy may be used to trick the brain into thinking both hands are receiving the same sensory input, potentially promoting recovery in the affected hemisphere. While mirror therapy is commonly used to promote motor recovery after stroke, similar principles can potentially aid in recovering sensory processing and perception.
These exercises are most effective when practiced consistently at home in addition to in-clinic therapy. Tools like therapy putty, textured blocks, or adaptive rehabilitation devices can be helpful.
Learn more about the MusicGlove from Flint Rehab for multi-sensory training in a music-based game!
4. Assistive Technology
Technology can provide crucial support for those with tactile agnosia, helping them complete tasks more efficiently and safely, especially in situations where recognizing an object by touch alone isn’t reliable.
Helpful assistive devices and tools for tactile agnosia include:
- Visual scanning tools: Devices, such as smart glasses, that identify objects using image recognition technology, even when they are unable to be easily seen (such as when looking for something in the dark)
- Smart home assistants: Voice-activated systems like Alexa or Google Home allow users to control lights, appliances, and calendars without handling multiple devices
Incorporating assistive tech into daily routines not only boosts independence but also reduces anxiety and the need for constant supervision.
Long Term Outlook for Patients With Tactile Agnosia: Can You Recover?
The outcome for someone with tactile agnosia depends largely on the cause and severity of brain damage. For those with mild impairment or recovering from stroke, improvements are possible, especially with consistent therapy. Here is a brief overview of the different factors that can affect the long term outlook for patients with tactile agnosia.
Factors Affecting Recovery for Tactile Agnosia:
- Age and overall health – Younger, healthier individuals often respond better to therapy.
- Severity and location of brain injury – More extensive damage can slow or limit recovery.
- Therapy adherence – Regular participation in rehabilitation programs improves outcomes.
- Support systems and resources – Access to caregivers, therapists, and adaptive tools plays a major role.
While full recovery may not always be achievable, many individuals learn to adapt and regain independence through structured rehabilitation.
Tactile Agnosia Frequently Asked Questions (FAQ)
Can tactile agnosia affect both hands?
Yes, it can, but this depends on the location and extent of the brain injury. In many cases, tactile agnosia affects only one hand, especially when the damage is limited to one hemisphere of the brain, such as after a stroke. However, if the injury involves areas on both sides of the brain, both hands may be affected.
Is tactile agnosia the same as numbness?
No, they’re very different. People with tactile agnosia can feel objects including their texture, size, weight, and temperature but cannot recognize or identify them by touch alone. In contrast, numbness involves reduced or lost sensation, where the person may not feel the object at all.
Can it go away over time?
Sometimes, yes. If the cause is a stroke, mild brain injury, or temporary swelling, partial or even significant recovery is possible, especially with early and consistent therapy. The brain can sometimes retrain itself through neuroplasticity, allowing other areas to compensate for the damage. However, recovery varies, and not everyone regains full function
Who treats tactile agnosia?
Diagnosis is usually made by a neurologist, who identifies the cause and extent of the brain injury. Treatment often involves a team-based approach, including occupational therapists to improve touch-based recognition skills and rehabilitation specialists who design exercises and strategies to help patients adapt in daily life. In some cases, neuropsychologists may also be involved to address cognitive and perceptual challenges.
Tactile Agnosia: Final Thoughts
Tactile agnosia may be uncommon, but for those living with it, the effects can be deeply personal. Understanding the condition is the first step toward managing it effectively.
With the right support, therapy, and adaptive tools, people with tactile agnosia can continue to engage in meaningful daily activities and maintain their quality of life.
Good luck!