When it comes to spinal cord conditions, few demand the urgent attention that cauda equina syndrome requires. This rare but serious condition affects the bundle of nerves at the base of your spinal cord, and recognizing its symptoms can make the difference between full recovery and permanent complications.
If you’ve been experiencing unusual back pain combined with other concerning symptoms, understanding cauda equina syndrome could be crucial.
In this article, we will take a look at cauda equina syndrome, common causes and symptoms, plus how to manage and treat this rare spinal cord condition.
What Is Cauda Equina Syndrome
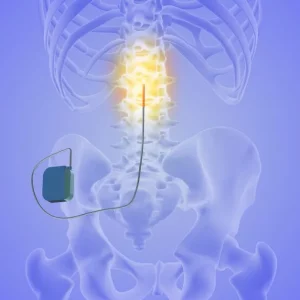
Cauda equina syndrome happens when a bundle of nerves at the base of the spine becomes compressed. These nerves control movement and sensation in the legs and play a critical role in bladder, bowel, and sexual function.
Because these functions are so central to daily life, even short periods of pressure on the cauda equina nerves can lead to serious consequences. This is why cauda equina syndrome is considered a medical emergency rather than a routine spine condition.
For many people, the diagnosis comes suddenly. Others may spend days or weeks noticing subtle changes before realizing something is seriously wrong. Both experiences are valid, and neither means the outcome is predetermined.
Understanding the Cauda Equina
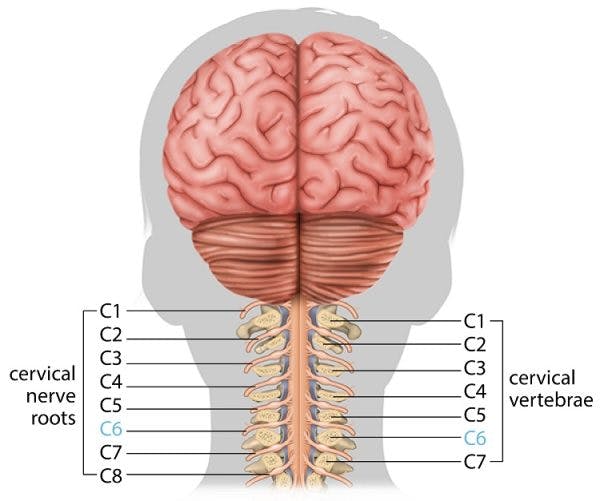
Before we discuss the syndrome itself, it helps to understand what the cauda equina actually is.
Where the Cauda Equina Is Located
The spinal cord does not extend all the way down the spine. It usually ends in the upper lumbar region. Below that point, the spinal canal contains a collection of nerve roots that branch downward. This bundle is called the cauda equina, named after its resemblance to a horse’s tail.
These nerves are responsible for:
- Moving the hips, knees, ankles, and feet
- Sending sensation from the legs and groin to the brain
- Controlling bladder and bowel function
- Supporting sexual sensation and response
When these nerves are healthy, communication between the brain and lower body feels automatic. When they are compressed, those signals can weaken or stop altogether.
Why Compression Causes Such Serious Symptoms
Nerve tissue is sensitive and does not tolerate pressure well. Unlike muscles, nerves cannot simply push through discomfort. When compression reduces blood flow or disrupts signaling, symptoms can appear quickly.
This is why cauda equina syndrome can progress from back pain to bladder or bowel changes in a short period of time. The condition is not dangerous because it is rare, but because of how much it can affect independence and quality of life if treatment is delayed.
What Causes Cauda Equina Syndrome?
Several conditions can lead to compression of the cauda equina nerves. The most common cause is a large herniated disc in the lumbar spine. When the soft center of a spinal disc pushes through its outer layer, it can press against the nerve bundle and create problems.
Other potential causes include:
- Spinal stenosis, where the spinal canal narrows over time
- Tumors growing in or near the spinal canal
- Infections or inflammation affecting the spine
- Traumatic injuries from accidents or falls
- Spinal bleeding (hematoma) that creates pressure
- Complications from spinal surgery
- Birth defects affecting spinal development
In some cases, the compression develops gradually over time. In others, it happens suddenly following an injury or acute disc herniation. Regardless of the cause, the pressure on these nerves creates an emergency situation that requires prompt intervention.
Symptoms of Cauda Equina Syndrome
Symptoms of cauda equina syndrome can vary, but they often involve a combination of pain, weakness, numbness, sexual dysfunction, and changes in bladder or bowel control. Not everyone experiences every symptom, which can make early recognition challenging.
Let’s take a look at some of the most common symptoms of cauda equina syndrome.
Lower Back Pain That Feels Different
Many people report severe lower back pain that feels deeper or more intense than typical back pain. The pain may spread into one or both legs and may worsen when standing or walking.
Leg Weakness or Sensory Changes
Weakness in the legs can make walking feel unstable or exhausting. Some people notice numbness, tingling, or a heavy sensation in the feet or calves. These changes may start on one side and spread.
Saddle Area Numbness
Reduced sensation in the inner thighs, buttocks, or groin is a key warning sign. This area is often described as the saddle region. Changes here are especially concerning and should never be ignored.
Bladder and Bowel Changes
Changes in bladder or bowel function are among the most alarming symptoms and often prompt people to seek care. These may include:
- Trouble starting urination
- Inability to fully empty the bladder
- Loss of bladder or bowel control
- Reduced awareness of bladder fullness
Depending on the extent that bladder function is affected, individuals may have incomplete cauda equina syndrome (abbreviated as CESI) or cauda equina syndrome with painless bladder retention (CESR).
Those with CESI may have difficulties with voiding, but still are able to do so voluntarily. Alternatively, in individuals with CESR, bladder control is completely lost, resulting in urine retention and painless overflow. This also signifies a more severe compression of the cauda equina.
Sexual Function Changes
Reduced sensation or changes in sexual response can occur due to nerve involvement. These symptoms are often difficult to talk about, but they are medically important and should be shared with a provider.
In fact, sexual dysfunction is one of three core symptoms that may signify the presence of cauda equina. According to Fraser’s group, who provided a frequently referenced standardized definition of cauda equina syndrome, individuals must have one or more of the following symptoms to be diagnosed with cauda equina syndrome:
- Bladder and/or bowel dysfunction
- Reduced sensation in the saddle area
- Sexual dysfunction
As mentioned above, many individuals experience a combination of these symptoms, along with back pain, leg pain, or limited motor/sensory function of the lower body.
Why Time Matters So Much With Cauda Equina Syndrome
Cauda equina syndrome is considered a surgical emergency because permanent nerve damage can occur if treatment is delayed. Nerves are sensitive structures, and prolonged compression can cause irreversible injury.
Research suggests that outcomes improve significantly when decompression surgery happens within 48 hours of symptom onset. Some studies indicate that surgery within 24 hours leads to the best recovery of bladder function and other affected areas.
The longer the nerves remain compressed, the higher the risk of permanent complications. These can include chronic pain, permanent weakness, ongoing bladder or bowel problems, and sexual dysfunction. Given the potential for lasting impact on quality of life, treating cauda equina syndrome as an emergency is essential.
How Doctors Diagnose This Condition
When you arrive at the emergency room with suspected cauda equina syndrome, doctors will move quickly to confirm the diagnosis. The process typically begins with a detailed discussion of your symptoms and a physical examination.
During the exam, your doctor will test your reflexes, muscle strength, and sensation in your lower body. They’ll check for saddle anesthesia and assess your ability to control your bladder and bowel, and may ask about any catheter use. A rectal examination helps determine whether you have normal sensation and muscle tone in that area.
The gold standard for diagnosing cauda equina syndrome is magnetic resonance imaging (MRI). This scan provides detailed images of your spine, clearly showing any compression of the nerve bundle and identifying the underlying cause. If MRI isn’t available or you can’t have one due to medical reasons, a CT myelogram might be used instead.
In some cases, additional tests like bladder function studies might be performed to assess the extent of nerve involvement.
Treatment Options for Cauda Equina Syndrome
Emergency Surgical Decompression
Most cases require urgent surgery to relieve pressure on the nerves. The goal is to restore space in the spinal canal and protect remaining nerve function.
Common procedures include removal of disc material, bone, tumors, or infected tissue. Timing matters, and earlier intervention is generally associated with better outcomes.
Medications and Supportive Care
Medications may be used alongside surgery to reduce inflammation, treat infection, or manage pain. On their own, medications are rarely enough when nerve compression is severe.
Recovery After Cauda Equina Syndrome
Recovery looks different for everyone. Some people notice improvements quickly, while others recover more gradually over months or longer. Generally, individuals with CESI have better recovery outcomes than those with CESR, although there are a number of other factors that can affect recovery.
Early Recovery Phase
Pain often improves first. Numbness, weakness, or bladder symptoms may take longer to change. Swelling around the nerves can temporarily mask improvement.
Long Term Nerve Healing
Nerves heal slowly. Progress may continue for a year or more. Small improvements over time can add up, even if recovery does not feel dramatic day to day.
Rehabilitation and Therapy
Rehabilitation helps people regain function and confidence. This may include:
- Physical therapy for strength and walking
- Occupational therapy for daily activities
- Pelvic floor therapy for bladder and bowel control
- Emotional support or counseling
Consistency and patience are important parts of this process.
Living With Long-Term Effects
For some individuals, complete recovery isn’t possible despite prompt treatment. Learning to manage ongoing symptoms becomes part of daily life. Bladder problems might require intermittent catheterization or other management strategies. Bowel issues may need dietary modifications and scheduled routines.
Mobility aids, from canes to wheelchairs, might be necessary if leg weakness or sensation deficits persist. Physical and occupational therapy can help you adapt and maintain the highest possible level of independence.
Support groups and counseling can provide emotional support as you adjust to any permanent changes. Many people find that connecting with others who have experienced cauda equina syndrome helps them cope with the challenges.
The Bottom Line
Cauda equina syndrome, while rare, represents a true medical emergency that requires immediate attention. The combination of severe back pain with bladder dysfunction, saddle numbness, or progressive leg weakness should always prompt an urgent visit to the emergency room.
Quick diagnosis and treatment offer the best chance for full recovery and help prevent permanent complications that can significantly impact your quality of life. If you or someone you know experiences symptoms suggesting cauda equina syndrome, don’t wait to see if things improve. Seek emergency medical care right away.
Understanding this condition empowers you to recognize warning signs and take action when it matters most. While cauda equina syndrome is uncommon, knowing what to watch for could make all the difference in protecting your long-term health and function.