Regaining bladder control after spinal cord injury may or may not be possible depending on the severity of your injury.
About 80% of spinal cord injury patients experience some loss of bladder control due to nerve damage, also known as neurogenic bladder dysfunction.
This article will explain why bladder dysfunction is so common after a spinal cord injury and discuss various scenarios where bladder control can return.
What Causes Loss of Bladder Control After Spinal Cord Injury?
The spinal cord transmits messages between the brain and body. However, after a spinal cord injury, messages may not be able to get past the site of injury, resulting in paralysis and loss of sensation below your level of injury.
Many people lose control of bladder functions after a spinal cord injury because the bladder muscles are innervated by some of the lowest nerve segments of the spinal cord. Damage to the spinal cord not only affects functions at the injury site but can also affect all functions below.
The reason why some spinal cord injury patients have normal bladder functions is because they have incomplete SCIs, which means some connections were not damaged by the injury. As a result, they may have some preserved motor control and sensation below their level of injury.
Next, we’ll discuss different types of neurogenic bladder dysfunction that can result from spinal cord injury.
Understanding the Different Types of Neurogenic Bladder Dysfunction
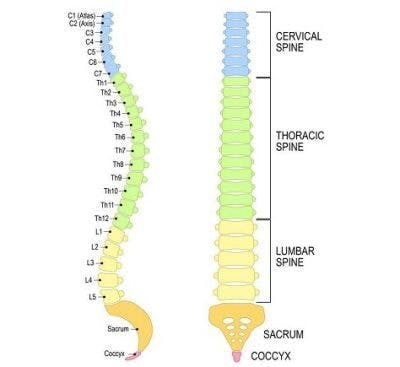
Two types of neurogenic bladder dysfunction can occur after a spinal cord injury: suprasacral and sacral.
Because bladder functions are innervated by the sacral region, damage at or below the sacral nerves will result in different outcomes than damage above.
Suprasacral Bladder Dysfunction
Suprasacral bladder dysfunction occurs after cervical, thoracic, or lumbar spinal cord injuries (areas above the sacral region).
This type of bladder dysfunction results in a spastic bladder (meaning the bladder reflex is essentially ‘over-active’ and the bladder may involuntarily contract without warning). This can cause urge incontinence, where individuals are not able to control their bladder functions.
When the bladder fills up, the increased pressure sets off a reflex, causing the sphincter to relax and involuntarily release urine, however emptying is often incomplete. Additionally, individuals with this condition may feel like they need to use the bathroom even when their bladder is not full.
In other words, due to impaired communication between the brain and the bladder and an over-active bladder reflex, individuals with injuries above the sacral region are often prone to bladder-related accidents.
Sacral Bladder Dysfunction
If your spinal cord injury occurs in the sacral region, it directly affects your bladder reflex and denervates the sphincter, causing flaccid bladder.
Flaccid bladder is characterized by low muscle tone. The detrusor (a muscle of the bladder that normally contracts to push urine out) is an extremely flexible muscle; however, when it is relaxed, it can cause the bladder to retain lots of urine and ultimately become too full. With this condition, when the bladder gets too full, it will then overflow causing accidents (overflow incontinence).
Poorly managed neurogenic bladder dysfunction can cause more serious complications including:
- Urinary tract infections
- Hydronephrosis (kidney swelling due to urine build-up)
- Kidney stones or urinary calculi
- Bladder cancer
In other words, due to lack of muscle tone, the bladder muscles remain in a relaxed and expanded state. As a result, the bladder can store more urine, which can be harmful because holding urine for too long can increase your risk for infections or kidney complications.
In the following section, we’ll discuss why loss of bladder control may be most severe immediately after a spinal cord injury.
Why Some People Regain Bladder Function Relatively Quickly
For some, loss of bladder control can be temporary. After a spinal cord injury, you may experience the temporary and complete loss of reflexes below your level of injury called spinal shock.
This is primarily caused by reduced blood supply and inflammation. Blood is rich in oxygen and nutrients that are essential for cellular activity. Excessive swelling in the spinal cord can decrease blood flow by up to 80%, causing major bodily functions to dysfunction.
Fortunately, spinal shock is a temporary condition that can last anywhere from a few days to several months. Once inflammation of the spinal cord starts to die down, functions below the level of injury may gradually start to return.
But is it possible to regain bladder control after spinal shock subsides?
Is Regaining Bladder Control After Spinal Cord Injury Possible?

Every spinal cord injury is unique, but as long as spared neural pathways exist at the site of injury (meaning it is an incomplete injury), regaining bladder function may be possible.
Spared neural pathways refer to undamaged connections at the location of injury that allow for communication between the brain and areas below the level of injury. They provide hope for recovery because they are capable of utilizing neuroplasticity, the central nervous system’s ability to rewire itself.
By consistently stimulating the spinal cord through task-specific practice, individuals may be able to improve weakened functions. The more spared neural pathways exist, the better the potential for recovery.
While regaining bladder function after spinal cord injury cannot be guaranteed, there are many ways to effectively manage neurogenic bladder dysfunction and improve your quality of life.
Bladder Management After Spinal Cord Injury

Proper management of neurogenic bladder dysfunction is essential for optimizing quality of life after spinal cord injury.
Management interventions primarily focus on emptying the bladder before it gets too full, however the specifics of a bladder intervention program will depend on the location of the injury.
Catheterization is the most common form of bladder management after SCI. It involves inserting a narrow tube into the body to drain urine from the bladder.
There are two main types of catheterization:
Intermittent catheterization requires using a catheter every 4-6 hours to empty the bladder. If you prefer not to be connected to a catheter all the time, this method is ideal.
Indwelling catheterization involves being connected to a catheter at all times. This method brings higher risk of a UTI, and is typically only used if there is a specific reason the individual cannot perform intermittent catheterization.
Alternative bladder management interventions include:
- Electrical stimulation involves implanting an electrode array to the bottom of the spine. The device emits electric currents below the site of injury to excite the neurons and enhance motor function.
- Anticholinergic medications are often the first line of treatment for overactive bladders because they can block chemicals that cause muscle contractions, which helps increase bladder capacity and reduce bladder pressure.
- Bladder augmentation surgery enlarges the bladder walls so individuals don’t have to empty the bladder so frequently.
- Botox injections can temporarily denervate spastic bladder muscles to increase bladder volume and relieve high bladder pressure.
Depending on your lifestyle and the severity of symptoms, some management interventions will be more ideal than others. Talk to your doctor to see which treatments will be best for you.
Regaining Bladder Control After Spinal Cord Injury: Key Points
Loss of bladder control is one of the most common outcomes of spinal cord injury. While it might be possible to improve bladder control, the outcomes of every SCI are different.
Learning to manage bladder problems is essential to avoid accidents and prevent further complications from developing.
Hopefully, this article helped you better understand how spinal cord injury can affect bladder functions and how to manage complications to improve your quality of life.