A stroke happens when blood flow to the brain gets interrupted—either from a blockage or bleeding—and it’s always a medical emergency. Without enough oxygen and nutrients, brain cells can start to die within minutes. But not all strokes are the same. The type of stroke can play a big role in how it’s treated and what recovery might look like.
In this guide, we’ll break down the main types of strokes, what causes them, and how they differ—so you can spot the signs early, get the right care, and take steps to stay healthy.
What Are the Main Categories of Stroke?
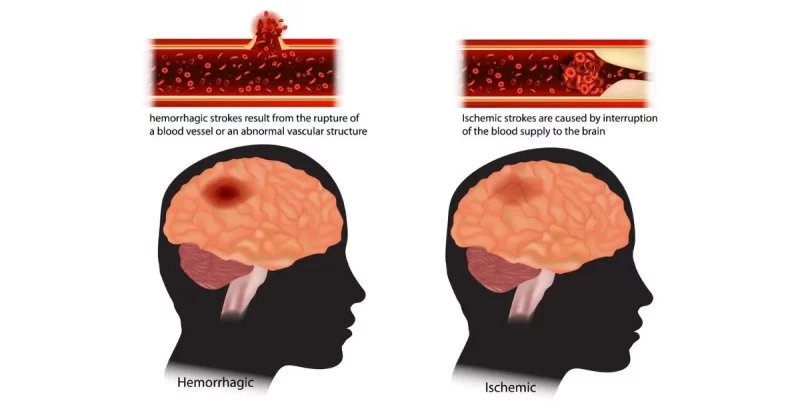
While all strokes involve a disruption in blood flow to the brain, not all strokes are the same. They’re generally divided into two main types based on what causes that disruption:
- Ischemic strokes are the most common, caused by a blockage in a blood vessel. They account for about 87% of all strokes.
- Hemorrhagic strokes are less common and occur when a blood vessel ruptures, leading to bleeding in or around the brain. These make up roughly 13% of cases.
Within each of these categories are several subtypes, each with its own causes, symptoms, and treatment approaches. Let’s break them down!
Different Types of Stroke: Breaking Down the 4 Types of Strokes
Ischemic Stroke
An ischemic stroke happens when a blood vessel that carries oxygen-rich blood to the brain gets blocked. When that blood can’t reach certain areas, brain cells start to get damaged and may eventually die without swift medical intervention.
Ischemic strokes can be further divided into 2 groups depending on how the clots occur. Let’s take a closer look at thrombotic and embolic strokes.
1. Thrombotic Stroke
A thrombotic stroke occurs when a blood clot (or thrombus) forms directly in one of the arteries supplying blood to the brain. This is often linked to atherosclerosis, a condition where fatty deposits build up in the arteries, narrowing them over time. High cholesterol, diabetes, and smoking can all increase the risk.
These strokes tend to develop gradually and may even go unnoticed at first. Symptoms often occur during sleep or early in the morning, and they can progress over hours or days.
A few examples of a thrombotic stroke can include:
Large Artery Thrombosis (Large Vessel Occlusion): This occurs in major arteries like the carotid or vertebral arteries, usually due to plaque buildup from atherosclerosis.
Small Vessel Disease (Lacunar Stroke): Lacunar strokes affect small, deep brain arteries and are linked to chronic high blood pressure or diabetes.
Watershed Stroke: Occurs in areas between large cerebral arteries—often triggered by a drop in blood pressure or cardiac arrest.
2. Embolic Stroke
An embolic stroke happens when a blood clot or other debris forms in another part of the body—often the heart—and travels to the brain through the bloodstream. Once it reaches a narrower artery, it can get lodged, blocking blood flow.
This type of stroke usually comes on suddenly, with no warning signs. A common underlying condition is atrial fibrillation, an irregular heart rhythm that increases the chance of clot formation in the heart.
A few examples of an embolic stroke can include:
Cardioembolic Stroke: Originates from the heart—commonly due to atrial fibrillation, heart failure, or heart valve disease.
Paradoxical Embolism: A venous clot passes to the arterial system through a heart defect (e.g., patent foramen ovale – PFO) and travels to the brain.
Artery-to-Artery Embolism: A clot from a large artery (like the carotid) breaks off and lodges in a smaller brain artery.
Hemorrhagic Stroke
A hemorrhagic stroke happens when a blood vessel in the brain bursts, causing bleeding either in the brain itself or in the space around it.
While these strokes aren’t as common, they tend to be more serious and can be life-threatening. There are two main types you’ll hear about: intracerebral hemorrhage (bleeding within the brain) and subarachnoid hemorrhage (bleeding in the space around the brain). Let’s explore what sets them apart.
3. Intracerebral Hemorrhage
An intracerebral hemorrhage is a type of stroke that happens when a blood vessel inside the brain bursts, causing bleeding directly into the brain tissue. This sudden rush of blood can damage brain cells and increase pressure inside the skull, making it a serious medical emergency.
One of the most common causes is long-term high blood pressure, which can quietly weaken blood vessel walls over time until they eventually give way. Other possible triggers include head trauma, certain blood disorders, or the use of blood-thinning medications.
Examples of intracerebral hemorrhage may include:
Hypertensive Hemorrhage: Typically affects deep brain structures like the basal ganglia and thalamus.
Lobar Hemorrhage: Occurs in the outer lobes of the brain; often linked to cerebral amyloid angiopathy.
Cerebellar Hemorrhage: Involves the cerebellum, leading to coordination problems, vomiting, and balance issues.
Brainstem Hemorrhage: Affects vital functions such as breathing, consciousness, and heart rate.
4. Subarachnoid Hemorrhage
A subarachnoid hemorrhage occurs when there’s bleeding in the space between the brain and the thin layers of tissue that cover and protect it—known as the subarachnoid space.
This type of stroke often feels sudden and intense, with many people describing it as the “worst headache of their life.” It’s usually caused by a ruptured aneurysm (a weakened, bulging area in a blood vessel), though head injuries can also be to blame.
Because the bleeding puts pressure on the brain and can interrupt normal circulation, quick medical attention is critical. While less common than other strokes, subarachnoid hemorrhages are serious and require urgent treatment.
Examples of a subarachnoid hemorrhage include:
Aneurysmal SAH: Caused by a ruptured cerebral aneurysm; often presents as a sudden, severe headache.
Non-Aneurysmal SAH: Also called perimesencephalic SAH, typically has a better outcome and is not due to aneurysm rupture.
AVM-Related Hemorrhage: Triggered by the rupture of an arteriovenous malformation—a congenital tangle of abnormal blood vessels.
How Stroke Type Affects Treatment
The type of stroke a person experiences has a direct impact on treatment strategy. Here’s a quick overview:
- Ischemic strokes are typically treated with clot-busting drugs (like tPA or TNK) or mechanical removal of the clot (thrombectomy), but only within a certain time window.
- Hemorrhagic strokes may require surgery or other procedures to stop the bleeding and relieve pressure on the brain.
- TIAs or mini strokes are a warning sign and often lead to lifestyle and medication changes to prevent a future stroke.
Correct diagnosis—usually confirmed by brain imaging such as a CT scan or MRI—is essential for guiding treatment and improving outcomes.
Final Thoughts: Understanding Stroke to Improve Outcomes
Stroke is a leading cause of disability and death worldwide. By understanding the different types—ischemic, hemorrhagic, and TIA—you’re better equipped to recognize the warning signs, advocate for timely care, and take steps to protect your brain health.
Each stroke is unique, and recovery often depends on how quickly treatment begins and how much damage occurs. But early action can save lives and improve quality of life.