No products in the cart.
No products in the cart.
No products in the cart.
No products in the cart.
Home » Neurological Recovery Blog » Stroke » Basal Ganglia Stroke: Understanding the Effects & Recovery Process
Last updated on October 10, 2023
Basal ganglia stroke is a rare type of stroke that can lead to unique long-term effects. These effects can include movement impairments, emotional blunting, and the loss of spontaneous speech. While a stroke in the basal ganglia may be accompanied by these negative effects, there is hope for recovery through dedicated rehabilitation.
In this article, you will learn about the potential long-term effects of basal ganglia stroke. We will also discuss how these secondary effects can impact a survivor’s independence and daily function. Then, you’ll learn how recovery is possible and what steps you can take to make the most of your rehabilitation journey.
Feel free to use these jump links to help you navigate this article:
A stroke occurs when the supply of blood in the brain becomes compromised. This happens when an artery becomes blocked, which is an ischemic stroke, or when an artery bursts, referring to a hemorrhagic stroke. Although a blockage and a bleed are different stroke mechanisms, both lead to a similar outcome – tissue damage within the brain. This can affect any area of the brain, including the basal ganglia.
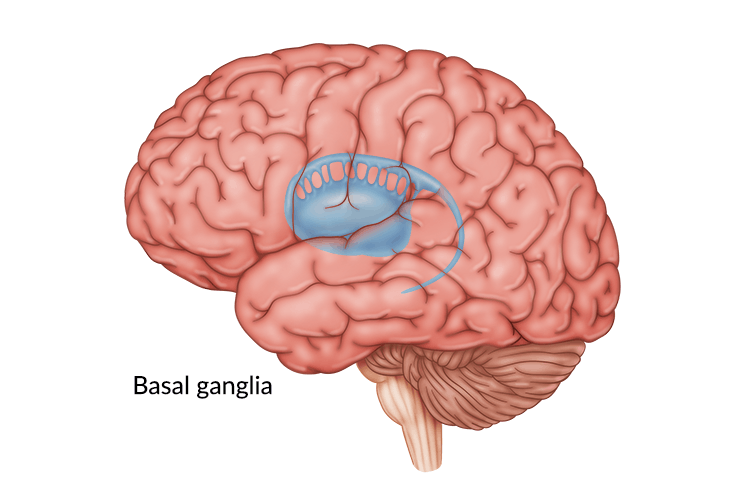
The basal ganglia are a group of structures that lie deep within the brain. These clusters of neurons are strongly connected with the cerebral cortex, thalamus, and brain stem. One type of ischemic stroke that affects these deep areas of the brain, including the basal ganglia, is called a lacunar stroke. However, while ischemic strokes are generally more common, many basal ganglia strokes are hemorrhagic due to the delicate nature of the blood supply deep in the brain.
A group of arteries called the circle of Willis provides oxygen-rich blood to structures deep in the brain like the basal ganglia. High blood pressure, also called hypertension, can cause a rupture in this blood supply, resulting in a stroke. Unfortunately, the impact of this tissue damage can lead to a wide array of secondary effects. This is because the basal ganglia are most associated with these functions:
When the basal ganglia are damaged due to stroke, any of these functions may be affected. It’s important to know that every stroke is different, so everyone will experience different secondary effects. Let’s dive deeper into the potential secondary effects of basal ganglia stroke in the next section.
The basal ganglia play a role in motor, cognitive, and even emotional functions. For this reason, the effects of this type of stroke are not always straightforward. The following effects are not guaranteed to occur after this type of stroke and may not occur at all. Instead, this list provides a general overview of the potential aftermath of basal ganglia stroke.
One of the primary functions of the basal ganglia is voluntary muscle control. When this control is compromised, it can lead to difficulty coordinating body movements. Therefore, motor impairments are one of the most common long-term effects of basal ganglia stroke.
Many types of motor impairments can occur, like dystonia and chorea. These conditions cause a survivor to demonstrate movements that appear random, fidgety, or irregular. In addition to uncoordinated movements, severe basal ganglia stroke can even result in post-stroke paralysis.
These motor effects can have a major impact on a survivor’s independence, daily function, and even safety. When movements are uncoordinated, a survivor’s balance and ability to walk are often affected, increasing fall risk. Furthermore, weakness or paralysis of certain muscle groups can prevent survivors from participating in their normal activities, including the activities of daily living.
Want 25 pages of stroke recovery exercises in a PDF? Click here to download our free Stroke Rehab Exercise ebook now (link opens a pop up for uninterrupted reading)
When the basal ganglia are affected by stroke, many survivors experience changes in their emotions or personality. For example, one study examined how disorders of the basal ganglia can alter your perception and experience of emotion. Specifically, basal ganglia stroke is associated with emotional blunting.
Emotional blunting means that positive stimulus is perceived less positively, and negative stimulus is perceived less negatively. This creates a flattened or “blunted” emotional affect. Additionally, survivors of basal ganglia stroke may have increased difficulty with the recognition of faces or names as well as trouble interpreting the emotions of others.
While life after stroke may feel distressing sometimes, it could be perceived less negatively by a basal ganglia stroke survivor due to emotional blunting. If that’s the case, why is post-stroke depression a common long-term effect?
Strokes in the basal ganglia are more often associated with depression than other types of stroke, specifically when the left hemisphere of the brain is affected. This takes place because of an important physiologic reason. The basal ganglia play a major role in transmitting mood-regulating signals, which can be interrupted due to stroke. When these signals are disrupted, a survivor is at a much greater risk of developing depression.
This mood disruption can also be compounded by the major life changes that take place because of stroke. For example, a survivor may experience changes in physical function, independence, community participation, and even their living situation. For these reasons, many survivors find themselves navigating the stages of grief after stroke, adding to depression.
The basal ganglia are involved in processes that span multiple functional categories. As a result, many survivors experience changes in speech due to basal ganglia stroke. In one study, a basal ganglia stroke survivor was reported to have a slow verbal response time. He did not speak unless spoken to. However, when he did talk, his responses were fluent and appropriate.
This reflects how a stroke in the basal ganglia may impair speech functions, particularly with voluntary speech. In addition, those affected by basal ganglia stroke may experience cognitive changes like poor attention, memory, or naming abilities. However, all strokes are different, so basal ganglia stroke effects will vary from survivor to survivor.
Most speech difficulties after stroke are categorized under a condition called aphasia. There are many different types of aphasia, and a speech-language pathologist can help diagnose and treat your specific condition.
Some survivors affected by basal ganglia stroke may experience numbness or reduced sensation in the body parts affected by stroke. This reduced sensation can make motor impairments even more prominent. This is because the brain needs sensory feedback to understand the body’s location and produce coordinated movements.
One possible explanation for sensory issues after basal ganglia stroke is its proximity to the thalamus. The thalamus plays a large role in relaying sensory signals. Numbness after stroke is one of the most common secondary effects of thalamic stroke. In addition to its impact on movement, reduced sensation can decrease a survivor’s safety and increase the risk of further injury.
Regardless of what secondary effects you may experience, your healthcare team is here to help you recover. Your team of doctors and therapists will identify your unique effects and can work with you to create an effective rehab plan. Through dedicated rehab, you can improve your function and recover from basal ganglia stroke.
The prognosis after basal ganglia stroke is unpredictable and depends on the specific area affected, However, the brain is amazing and is capable of healing itself after neurological injury. This ability to restore function is thanks to a natural process called neuroplasticity. Neuroplasticity enables the brain to reorganize itself, create new pathways, and rearrange existing ones as a result of experience.
This means that the functions lost after stroke can be restored, partially or fully. When an area of the brain experiences injury due to stroke, this area loses function and this loss is sometimes permanent. However, the brain can rewire pathways for these functions in other healthy areas of the brain. This allows survivors to regain control of certain abilities previously lost due to stroke. For example, if a basal ganglia stroke survivor loses the ability to control their arm, neuroplasticity allows new areas of the brain to take on arm function.
While some recovery takes place automatically due to spontaneous recovery, progress generally slows around 3-6 months after stroke. Fortunately, you can improve function at any point of recovery (even years after stroke) through neuroplasticity.
Neuroplasticity requires hard work through experience to make lasting changes, which is the purpose of rehabilitation. During the stroke recovery process, survivors are exposed to intense, therapeutic experiences designed to encourage the brain to rewire itself and recover lost functions. While survivors will likely experience plateaus or even occasional regressions during their journey, progress is always possible.
Most stroke recovery treatments focus on activating neuroplasticity to encourage the brain to rewire itself. Neuroplasticity is activated by experience, especially when the experience is repetitive and consistent. This high repetition is sometimes referred to as massed practice and is crucial for rehab. Now, let’s discuss some of the best therapies for basal ganglia stroke recovery that survivors may encounter.
Remember that repetition is the key to recovery. Providing the brain with repetitive stimulation allows you to target the areas you want to improve. With time, the brain’s natural rewiring process can allow you to recover function and improve your quality of life after basal ganglia stroke.
Basal ganglia stroke is complex, but it is possible for survivors to restore important functions and improve performance of daily activities. This is especially true when a consistent rehabilitation plan is followed. By exposing the brain to repetitive stimuli, you can help spark neuroplasticity to rewire the brain and regain lost skills.
Even if recovery has slowed down, the brain will continue to respond to repetitive stimulation and you will see improvements once again. This is why working closely with your therapy team is so important. Your therapists will help you set meaningful goals and can help customize your plan to meet your current abilities. Then, it is up to you to put in the work.
We hope this article has helped explain basal ganglia stroke and the recovery journey. Although this type of stroke has unique effects, these can be improved through intentional rehab. Keep taking small steps toward recovery each day and you’ll be amazed at what you can accomplish.
Get our free stroke recovery ebook by signing up below! It contains 15 tips every stroke survivor and caregiver must know. You’ll also receive our weekly Monday newsletter that contains 5 articles on stroke recovery. We will never sell your email address, and we never spam. That we promise.


Do you have these 25 pages of rehab exercises?
Get a free copy of our ebook Full Body Exercises for Stroke Patients. Click here to get instant access.
“My name is Monica Davis but the person who is using the FitMi is my husband, Jerry. I first came across FitMi on Facebook. I pondered it for nearly a year. In that time, he had PT, OT and Speech therapy, as well as vision therapy.
I got a little more serious about ordering the FitMi when that all ended 7 months after his stroke. I wish I hadn’t waited to order it. He enjoys it and it is quite a workout!
He loves it when he levels up and gets WOO HOOs! It is a wonderful product! His stroke has affected his left side. Quick medical attention, therapy and FitMi have helped him tremendously!”
FitMi is like your own personal therapist encouraging you to accomplish the high repetition of exercise needed to improve.
When you beat your high score or unlock a new exercise, FitMi provides a little “woo hoo!” as auditory feedback. It’s oddly satisfying and helps motivate you to keep up the great work.
In Jerry’s photo below, you can see him with the FitMi pucks below his feet for one of the leg exercises:
Many therapists recommend using FitMi at home between outpatient therapy visits and they are amazed by how much faster patients improve when using it.
It’s no surprise why over 14,000 OTs voted for FitMi as “Best of Show” at the annual AOTA conference; and why the #1 rehabilitation hospital in America, Shirley Ryan Ability Lab, uses FitMi with their patients.
This award-winning home therapy device is the perfect way to continue recovery from home. Read more stories and reviews by clicking the button below:
Grab a free rehab exercise ebook!
Sign up to receive a free PDF ebook with recovery exercises for stroke, traumatic brain injury, or spinal cord injury below: