The anterior cerebral artery, called the ACA, is a vital source of blood flow within the brain. When an ACA stroke occurs, it interrupts blood flow and can cause a wide array of secondary effects. The effects of ACA stroke can encompass many aspects of daily life, impacting motor, sensory, and cognitive functions.
Fortunately, there is hope for recovery from ACA stroke through dedication to a consistent rehabilitation plan. In this article we will review the causes of ACA stroke, common symptoms, and rehabilitation techniques. To help you navigate through this article, you can use these jump links:
Causes of ACA Stroke
The anterior cerebral artery stems from the internal carotid artery and supplies oxygen-rich blood to the front of the brain, specifically to the frontal and parietal lobes. The ACA also supplies structures deep within the brain, such as the cingulate cortex and internal capsule.
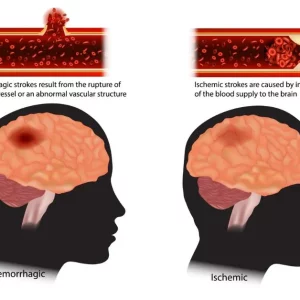
ACA stroke can occur due to two main types of interruption to the brain’s blood flow. An ischemic stroke occurs when blood flow within the artery is obstructed due to a blockage or clot. On the other hand, a hemorrhagic stroke occurs when an artery bursts or ruptures, causing uncontrolled bleeding within the brain.
ACA stroke is generally ischemic in nature and is most often a result of atherosclerosis, or a buildup of plaque within the walls of the artery. ACA stroke is very rare, making up just 0.3-4.4% of stroke cases. In comparison, a nearby artery called the middle cerebral artery is the most common artery affected by ischemic stroke. This is commonly referred to as mca stroke.
The anterior cerebral artery actually consists of a pair of connected arteries that supply different regions of the brain. For this reason, we divide the ACA into “left” and “right” sides. The left ACA and right ACA are responsible for delivering blood to their corresponding halves, or hemispheres, of the brain. Because of this separation, the specific branch of the artery affected largely determines the secondary effects of an ACA stroke.
Each hemisphere of the brain controls functions on the opposite side of the body. therefore, a left ACA stroke results in right-side deficits while a right ACA stroke causes left-side deficits. However, in many cases of ACA stroke, the damage affects both hemispheres of the brain.
ACA Stroke Symptoms
Since ACA stroke is uncommon, data regarding prognosis and general outcomes is limited. Additionally, the resulting symptoms of ACA stroke depend heavily on factors such as the specific area(s) affected, the severity of the stroke, and administration of timely medical intervention. However, we know this type of stroke can result in a variety of distinctive secondary effects due to the ACA’s crucial role in supplying blood to the frontal lobe, parietal lobe, and deep brain structures.
Here are some of the most common symptoms people experience with an ACA stroke.
Hemiparesis
Hemiparesis refers to weakness of one half of the body. It affects the side of the body opposite the hemisphere of the brain affected. For example, a right ACA stroke can result in left hemiparesis and vice versa. If both hemispheres are affected, it can cause weakness on both sides of the body.
Hemiplegia
Hemiplegia is more severe than hemiparesis and refers to paralysis of one half of the body. In ACA stroke cases, the leg is often more affected than the arm. Right hemiplegia refers to paralyzed muscles on the right side of the body following injury to the left hemisphere of the brain. Left hemiplegia refers to paralyzed muscles on the left side of the body after right hemisphere injury.
Behavioral Changes
Behavioral changes are another common symptom following an ACA stroke. Common changes in behavior after ACA stroke include apathy and feelings of indifference. Additionally, survivors of ACA stroke may demonstrate avoidance of social interaction.
Aphasia
ACA stroke can be accompanied by a variety of speech disorders including aphasia. Aphasia refers to difficulty producing or comprehending speech. Since the language center of the brain is located in the left hemisphere, aphasia is generally present following left ACA stroke.
Common types of aphasia include Broca’s Aphasia (expressive or non-fluent aphasia) and Wernicke’s Aphasia (receptive or fluent aphasia).
Sensory Deficits
Although less common than other symptoms, ACA stroke sometimes results in decreased sensation in areas such as the face, arm, and leg. In these cases, sensory reeducation can help to regain sensation.
Motor Apraxia
This refers to difficulty performing intentional movement despite having the desire to do so. This can include poor coordination and decreased control of the limbs, face, and tongue.
Urinary Incontinence
Incontinence, or a lack of urinary control, has been reported as a symptom in many cases of ACA stroke. This occurs as a result of tissue damage in areas of the brain responsible for bladder function, such as the frontal lobe. In addition to impaired neural communication, incontinence can be related to weakness of the muscles controlling the bladder following stroke.
Disconnection Syndrome
When ACA stroke affects the corpus callosum, the ability for the two hemispheres of the brain to communicate can become disrupted. This can lead to a condition known as disconnection syndrome, sometimes resulting in impaired body part recognition, communication deficits, and alien hand syndrome.
Diagnosis and Initial Treatment
Quick detection and timely treatment are crucial following the onset of ACA stroke. Faster response to stroke symptoms allows medical staff to provide life-saving treatments and minimize tissue damage within the brain. Stroke symptoms can include facial drooping, weakness of one side of the body, slurred speech, and sometimes headache. To help protect yourself or a loved one, take time to review these stroke warning signs.
Upon arrival to the hospital, an individual experiencing a suspected stroke will receive immediate treatment to stabilize their condition and address the cause of the stroke. Imaging such as MRI or CT can help pinpoint the type and location of the stroke. Additionally, doctors may administer medications such as tPA (tissue plasminogen activator) or TNK (tenecteplase) to restore normal blood flow.
In some cases, medication may not be sufficient and surgical intervention such as a mechanical embolectomy or thrombectomy is required to remove a clot from the ACA. Once doctors restore blood flow and stabilize the survivor, the road to recovery can begin!
ACA Stroke Rehabilitation
Although the secondary effects of ACA stroke tend to follow a common pattern, every individual is unique and will therefore require an individualized rehabilitation plan. Your therapy team is specifically trained to help you return to your normal daily activities as well as the hobbies you love.
The brain is resilient and is able to heal and rewire itself through a process called neuroplasticity. Through this process, areas of healthy brain tissue can take on the functions of areas of damaged tissue by creating and strengthening neural connections.
Neuroplasticity requires time, high repetition, and consistency, but will allow you to regain lost function as your recovery journey progresses. The more an exercise or skill is practiced, the stronger and more efficient the connections needed for that skill will become. Your rehab team will also provide you with a home exercise program so you can activate neuroplasticity and continue to make gains between therapy sessions.
Since ACA stroke can result in motor, sensory, and cognitive changes, your rehab plan will likely consist of several different therapy types and treatments. These therapies can include:
Physical Therapy
A physical therapist (PT) is a movement expert whose goal is to help you regain physical function. They can help address hemiparesis or hemiplegia by guiding you through weight-bearing activities and by utilizing treatments such as electrical stimulation. These interventions will help encourage muscle activation and the creation of neural pathways.
Physical therapists will tailor specific exercises to allow you to regain ROM, increase muscle strength, decrease spasticity, and reduce risk of developing muscle contractures after ACA stroke. They can also help you safely practice activities including walking, transfers, and bed mobility.
Speech Therapy
Speech therapy, provided by a speech-language pathologist (SLP), is an incredible resource following ACA stroke. Many survivors of ACA stroke experience aphasia and will require speech therapy to address motor function of the tongue, face, and lips through speech exercises. Speech therapists can assist with adaptive speech techniques and production of sounds as well as recommend equipment to allow you to better communicate with those around you.
Additionally, speech therapists can help address dysphagia, or difficulty swallowing after stroke. Dysphagia affects many stroke survivors and can lead to serious complications if not addressed. Your SLP will be able to create a customized treatment plan to meet your specific needs after ACA stroke.
Occupational Therapy
An occupational therapist (OT) is a vital part of your rehab team as they help you perform daily activities and promote independence in your environment. Your occupational therapist can work to reduce hand spasticity or curled fingers, provide education on appropriate hand or arm splints, and recommend adaptive equipment to increase efficiency with daily tasks.
An OT can guide you through sensory reeducation to help increase sensation after stroke and will also prescribe fine motor activities to address motor apraxia and decreased coordination. Just like physical and speech therapies, occupational therapy requires dedicated practice to see progress.
Psychological Care
In addition to physical effects, ACA stroke can be accompanied by behavioral and psychological changes. For this reason, mental and psychological health is a critical piece of the ACA stroke recovery process.
A licensed therapist can help you navigate the difficult feelings that accompany stroke, such as grief, loss, and anxiety. Additionally, depression is commonly experienced after stroke and should be taken seriously—which is why a therapist can be a valuable resource during your recovery journey.
Due to the location and function of the anterior cerebral artery, survivors may experience increased feelings of apathy, indifference, or social avoidance after ACA stroke. A therapist can help you identify these feelings and develop a strategy to address behavioral changes you may be experiencing due to ACA stroke.
Recovery from ACA Stroke
ACA stroke can affect one or both hemispheres of the brain and lead to a variety of motor, sensory, and cognitive secondary effects. This can include hemiparesis or hemiplegia, sensory deficits, behavioral changes, aphasia, and apraxia. Detection of stroke warning signs and timely medical intervention are vital to help reduce these secondary effects and maximize chances of recovery.
The road to recovery after ACA stroke will be full of highs and lows, but consistency and dedication will continue to yield results with time. Every stroke recovery timeline looks different, so it is important to stay focused on your own specific goals and to lean on support from your family, friends, and rehab team.
Although ACA stroke is uncommon and can impact many aspects of daily life, there is a wide variety of rehabilitation techniques available to address your specific needs and return you to the activities you love. We hope this article has helped you better understand the mechanism of ACA stroke, common symptoms, and the treatment options that are available to help you achieve your goals.