Autonomic dysreflexia is a condition characterized by sudden changes in autonomic functions such as blood pressure, heart rate, and body temperature. It most commonly occurs after spinal cord injuries (SCI) at the T6 level or higher; however, it may also occur in individuals with other types of neurological conditions.
If not properly managed, autonomic dysreflexia (AD) can be life-threatening. Fortunately, there are effective ways to avoid triggers and prevent the response from occurring.
To help you understand what autonomic dysreflexia is, this article will discuss:
What Causes Autonomic Dysreflexia?
The autonomic nervous system is responsible for regulating involuntary body functions such as blood pressure, breathing, body temperature regulation, and digestion. When an individual has autonomic dysreflexia, sudden changes in autonomic nervous system functions can be triggered.
Autonomic dysreflexia may occur following a spinal cord injury because the transmission of messages between the brain, spinal cord, peripheral nerves, and muscles is disrupted. As a result, potentially damaging (noxious) stimulation below the level of injury can set off a reflex that activates the sympathetic (fight or flight) portion of the autonomic nervous system, causing the blood vessels to constrict, which results in a spike in blood pressure.
During an episode of autonomic dysreflexia, the opposing portion of the autonomic nervous system, called the parasympathetic nervous system, is unable to appropriately counter this sympathetic reflex.
Usually, the brain sends messages throughout the body to inform you of what the noxious stimulus is so that you can remove it. For example, if you touch a hot object, your brain will immediately send signals to move away from it. When the stimulus is removed, the sympathetic nervous system’s fight or flight response is no longer needed, thus the brain sends signals to relax the blood vessels and reduce blood pressure.
However, after an SCI, messages from the brain may be unable to reach areas below one’s level of injury. As a result, the body may be unable to return to its normal state and remains in a state of dysreflexia (until the noxious stimulus is removed). This may put you at risk for other serious conditions such as brain injury, stroke, seizures, organ failure, and even death.
Now that you understand why autonomic dysreflexia occurs after spinal cord injury, let’s discuss who is at risk of developing it.
Who is at Risk for Developing Autonomic Dysreflexia?
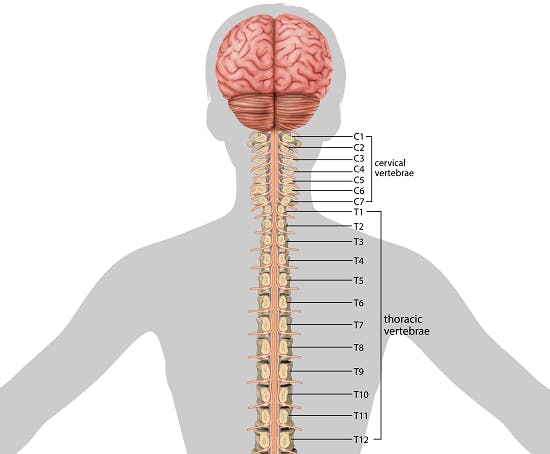
Not all individuals with spinal cord injuries are at risk for developing autonomic dysreflexia. It is most common following spinal cord injuries at the T6 level or higher. In fact, it’s suggested that about 50-70% of individuals with T6 or higher level spinal cord injuries experience symptoms of autonomic dysreflexia.
This means that individuals with cervical spinal cord injuries and high-thoracic spinal cord injuries are at the highest risk of AD. Although much rarer, it can also occur with injuries below the T6 level. However, it is unlikely to occur in individuals with spinal cord injuries below the T10 level.
Autonomic dysreflexia can occur in individuals with complete or incomplete spinal cord injuries. However, the more severe your injury, the greater the risk of developing AD.
Other causes of autonomic dysreflexia include:
- spinal cord tumors
- neurological surgery above the T6 level
- multiple sclerosis
- catecholamine secreting tumors
Up next, we’ll discuss what can trigger episodes of autonomic dysreflexia.
Triggers of Autonomic Dysreflexia
Nearly anything that bothers the body below one’s level of injury can cause autonomic dysreflexia. It’s not yet understood why some people experience AD more often than others, but all individuals with higher-level spinal cord injuries should be aware of potential triggers that can cause the autonomic nervous system to overreact.
Common triggers of autonomic dysreflexia include:
- Full bladders or blocked/full catheter bags
- Constipation or distended bowels
- Skin irritations (burns, cuts, bruises, pressure sores, etc.)
- Extreme temperatures
- Tight clothing
- Any sort of pressure on the body
- Menstrual cramps
- Sexual activity
Individuals with autonomic dysreflexia must keep an eye out for these triggers and try to avoid them as much as possible. In instances when individuals are unaware of triggers, signs of AD may occur. The sooner you’re able to identify these signs and symptoms, the sooner you can prevent the response from progressing.
Signs and Symptoms of Autonomic Dysreflexia

While the most common sign of autonomic dysreflexia is a sudden increase in blood pressure, there are many other ways the autonomic nervous system can react.
Depending on the severity of injury, level of injury, and pre-existing health complications, each individual may experience AD differently.
Common signs and symptoms of autonomic dysreflexia include:
- Severe headaches (this is one of the most common symptoms)
- Elevated blood pressure (typically 20-40 mm Hg above baseline in adults)
- Sweating above the level of injury
- Flushed or blotchy skin above the level of injury
- Slow heart rate (bradycardia) or fast heart rate (tachycardia)
- Anxiety or feelings of a panic attack
- Blurry vision
- Goosebumps above the level of injury
- Nausea
- Vomiting
- Tightness or pressure in the chest
- Stuffy nose
In the following section, we’ll review what SCI survivors should do if they notice signs of autonomic dysreflexia.
Treatment and Management of Autonomic Dysreflexia
Often, individuals with spinal cord injuries can manage their autonomic dysreflexia by avoiding triggers and staying alert for early signs.
In order to know if your blood pressure has spiked, it’s important to be aware of what your baseline blood pressure range typically is. Often, individuals with spinal cord injuries are hypotensive, meaning that they have low blood pressure. Therefore, a sudden rise in blood pressure resulting in a “normal” blood pressure reading may still suggest an episode of AD and require attention.
If you notice a sudden rise in blood pressure or any other signs of autonomic dysreflexia, make sure to immediately sit upright (in a safe, supported position), lower the legs, and keep your head raised to help lower your blood pressure. After that, it is crucial to identify what is triggering the reaction. Generally, AD will subside after the trigger is removed.
Some of the best practices for treating autonomic dysreflexia include:
- Emptying the bowel and bladder regularly (85% of AD episodes are related to bladder or bowel complications)
- Checking for clogs or kinks in catheters
- Wearing looser clothing (but not too loose because the excess fabric can bunch up)
- Avoiding hard or sharp objects in clothing that can rub again the skin such as zippers and pins
- Inspecting the skin daily for pressure sores, bruises, or other signs of irritation
- Avoiding extreme temperatures
Additionally, applying topical treatments such as nitroglycerin paste may help reduce hypertension and irregular heartbeats. Alternatively, doctors may prescribe oral medications such as nifedipine and nitrates to relieve signs of autonomic dysreflexia.
After taking the necessary actions to relieve signs of autonomic dysreflexia and removing the associated trigger, individuals should use a blood pressure cuff every 5-10 minutes to ensure that their blood pressure is stabilizing. If symptoms do not subside, seek immediate medical attention.
Understanding Autonomic Dysreflexia: Key Points
Autonomic dysreflexia is most common in individuals with T6 or higher-level spinal cord injuries. Because messages from the brain cannot reach areas below the level of injury, major body functions like blood pressure, heart rate, and temperature regulation may be disrupted. Therefore, it is essential to be alert for potential triggers and signs of AD to prevent symptoms from progressing.
We hope this article helped you understand what autonomic dysreflexia is, why it occurs, and how to manage it.