Brain stem stroke is a unique type of stroke that is uncommon, accounting for 10-15% of cases. While all strokes are unique, brain stem strokes are particularly different in terms of symptoms and recovery. This is because of the brain stem’s role in many of the body’s vital functions such as breathing, heart rate, and blood pressure regulation.
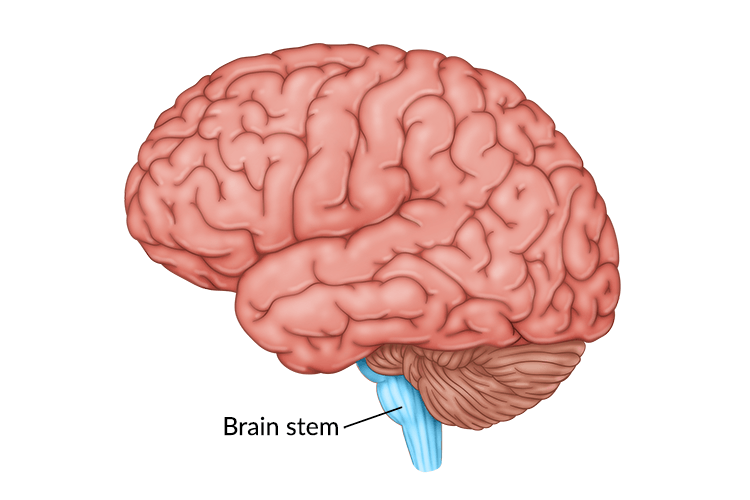
The brain stem is located at the base of the brain and connects the main cerebrum to the cerebellum and spinal cord. Due to its small size, many brain stem strokes are relatively small. However, the effects can be significant and, oftentimes, life-threatening. Fortunately, there is hope for survivors as intensive rehabilitation can help individuals regain function and independence.
In this article, we will outline the causes and secondary effects of brain stem stroke. Then we will discuss the rehabilitation process and the different components of recovery. Additionally, we will share stories from real brain stem stroke survivors to illustrate how others have overcome the challenges of this type of stroke.
To help you navigate this article, use the links below to jump straight to any section:
How a Stroke Affects the Brain Stem
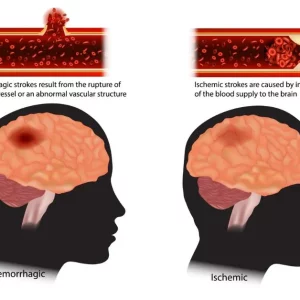
Two main types of stroke can affect the brain stem. The first, called ischemic stroke, takes place when the supply of blood becomes compromised by a clogged vessel. The second, called hemorrhagic stroke, occurs when a vessel bursts. Both types of stroke contribute to cell death and tissue damage in the brain stem due to the disruption of blood flow or the pressure caused by a hemorrhage. Ischemic strokes in the brain stem are more common than hemorrhagic and can sometimes be further classified as a lacunar stroke.
A stroke can occur in any of the three major areas of the brain stem: the midbrain, pons, and medulla. Furthermore, some strokes that injure the brain stem also affect the cerebellum (located behind the top part of the brain stem) or other surrounding areas. Of the three sections of the brain stem, the pons is most affected and is the site of tissue damage in 60% of brain stem stroke cases.
Risk factors that increase the likelihood of stroke include high blood pressure, high cholesterol, diabetes, and obesity. Additionally, smoking can increase the risk of stroke by 2-4 times. For this reason, it is important to manage risk factors to reduce the risk of a first or even a second stroke.
When a brain stem stroke occurs, it can cause atypical symptoms like vertigo, nausea, and headache. These can be present with or without the hallmark symptoms of a stroke, such as slurred speech or weakness of one side of the body. As a result of these unique symptoms, a brain stem stroke can be difficult to diagnose.
As with all strokes, this event is a medical emergency that requires swift treatment to save the person’s life. Take the time to familiarize yourself with the different warning signs of stroke to protect yourself or a loved one. Timely medical treatment is crucial to restore the body’s vital function and minimize tissue damage. After a stroke has been treated, the survivor must work to overcome the secondary effects that occur, which we will discuss next.
Potential Secondary Effects of Brain Stem Stroke
The brain stem plays a major role in vital body functions such as breathing, consciousness, and heart rate. Therefore, the secondary effects of a brain stem stroke can impact these functions and others. For this reason, a brain stem stroke can lead to a wide range of secondary effects that impact a survivor’s daily life and independence.
While strokes that affect other areas of the brain are often accompanied by motor or sensory impairments, the effects of a stroke in the brain stem may present somewhat differently. To help you better understand this, let’s discuss some of the possible secondary effects:
- Coma. The brain stem controls the state of consciousness, so a stroke in this area of the brain can result in a coma.
- Locked-in syndrome. This rare condition occurs when an individual is completely paralyzed but some of the muscles that control eye movement are spared. An individual affected by locked-in syndrome is generally conscious and able to think and reason, but is unable to move or speak due to injury to the brain stem.
- Difficulty breathing. Breathing is controlled by the medulla, which is part of the brain stem. A stroke in this area can affect the ability to breathe if automatic respiratory functions are disrupted.
- Dysphagia. Difficulty swallowing (a condition called dysphagia), is common after a brain stem stroke. This affects around 47% of survivors, but long-term outcomes are generally positive.
- Hemiparesis or hemiplegia. Like other types of strokes, brain stem stroke can lead to hemiparesis or hemiplegia. This refers to weakness or paralysis of one half of the body.
- Vision problems. Vision difficulties, such as nystagmus (when the eye makes repetitive, uncontrolled movements), can occur after a brain stem stroke.
- Ataxia. Ataxia refers to difficulty with voluntary motor control, often resulting in poor balance and uncoordinated movements of the limbs. This condition is specific to damage to the cerebellum and surrounding areas like the brain stem.
- Wallenberg’s syndrome. This rare condition encompasses many different secondary effects. Individuals affected by this syndrome often experience different symptoms on opposing sides of the body. For example, they may have numbness or weakness in their left arm and leg while also experiencing these same symptoms on the right side of the face.
- Loss of sensation. Sensory loss is common after injury to the pons. This can include loss of smell and taste as well as decreased sensation of the face. Additionally, some survivors may have difficulty sensing temperature and vibration or may experience numbness.
- Vertigo. Brain stem strokes are frequently accompanied by intense dizziness or the sensation that the environment is spinning. This can also be a warning sign of stroke in this area of the brain.
Outlook and Prognosis
Every stroke is different, and every survivor experiences stroke secondary effects differently. Some individuals may have solely sensory symptoms while others can experience the disruption of vital body functions due to brain stem stroke. If functions like respiration are affected, the survivor may require a ventilator to assist with breathing or other invasive interventions.
Since the brain stem plays such a major role in the body’s vital functions, the mortality rate for this type of stroke is relatively high. However, the rate of functional recovery is higher than in cases of hemispheric stroke. In fact, one study recorded that 35% of brain stem stroke survivors were able to return to independent living.
If a survivor participates in long-term rehabilitation, they can often regain significant function after stroke. While this does depend largely on the type of stroke the survivor experiences, there is always hope for recovery. In the next section, we will discuss what the rehabilitation process often looks like for survivors.
Rehabilitation for Brain Stem Stroke Patients
After the initial stay in the hospital, many stroke survivors spend time in inpatient rehabilitation. During this period, survivors will generally participate in 3-4 hours of therapy per day. The therapy team often includes physical, occupational, and speech therapists who work with survivors to regain lost functions.
For instance, if a stroke survivor struggles with loss of sensation (like numbness or difficulty with smell and taste), an occupational therapist can help them with sensory retraining. They can also help the survivor relearn how to perform activities of daily living such as bathing and dressing.
If the survivor is affected by locked-in syndrome, therapists can help the survivor accomplish passive range-of-motion exercises to stimulate the brain and prevent contractures. Additionally, a physical therapist can guide a survivor through exercises after stroke to increase strength, improve balance, and reduce muscle atrophy. This can allow the survivor to return to functional activities like walking and independent transfers.
Impairments like dysphagia or speech disorders can be addressed and treated with the help of a speech-language pathologist (also called a speech therapist). These trained professionals can help survivors regain the ability to swallow and provide speech exercises to improve the strength of their facial muscles. Furthermore, a speech therapist can offer tips to improve safety with eating to reduce the risk of aspiration pneumonia.
Retraining the Brain
One of the overarching goals during rehabilitation is to spark neuroplasticity: the brain’s ability to rewire itself. Neuroplasticity allows functions in affected areas of the brain to be rewired to healthier, unaffected areas. This growth of neural pathways is most active in the first 3-6 months after stroke and is responsible for what is known as spontaneous recovery.
Recovery requires hard work and consistency because neuroplasticity is activated through massed practice of therapy exercises. Regularly practicing the skills you want to improve will allow you to see the greatest improvements, even if progress is slow or you experience occasional plateaus.
While the fastest improvements may be seen in the initial 6 months, progress can be made months and even years after stroke. This means that, after discharge from inpatient therapy, stroke survivors must continue with rehabilitation both at home and at outpatient therapy.
To stay motivated and consistent, survivors can explore interactive neurorehabilitation devices that can be used at home. Additionally, it helps to hear the experiences of other brain stem stroke survivors to learn more about their rehabilitation journey. Recovery is highly unique, so keep this in mind when reading other survivors’ stories.
Brain Stem Stroke Survivor Stories
Flint Rehab has had the pleasure of speaking with various brain stem stroke survivors to learn about their experiences. To encourage you during your recovery journey, we would like to share a couple of those stories with you.
First, we’d like to share from Becky, who experienced a brain stem stroke at the end of November 2007. She was initially paralyzed from the neck down but is now able to move her body again. Not all patients will recover from locked-in syndrome like Becky, but she shows that recovery is possible. Check out her story in the video below:
Next, we spoke with a stroke survivor named Luke, who experienced a brain stem stroke in July 2019. Here’s what he said:
I was in a coma for six days. Some people thought I was never going to wake up. And I wasn’t supposed to. But I did, and I’ve been recovering ever since. I had to re-learn everything. How to walk, how to talk, how to eat, basic human functioning. I was confined to a wheelchair for two months, and I learned how to walk again with an AFO around my left leg, which I actually got removed a couple months ago.
They discharged me from the hospital in September 2019, and I’ve been doing outpatient therapy ever since. As of right now, I have a job, and my doctors have cleared me to take some online college classes to prepare me for my return to college.
My rehab consisted of three different kinds of therapies: physical, occupational, and speech. I’ve been doing rehab for over a year now, and it started a couple days after I got out of the hospital. As of right now, I have graduated from all therapies and have taken an intense neuro-psych evaluation (which I didn’t do so well on), which was going to clear me for college, but it didn’t.
But all in all, I’ve been participating in rehab for over a year now, as brain stem injuries take a long time to heal (so I’ve learned). I wanted to share my story so that people can learn from it and never give up on anything, because if you do, you’re only holding yourself back from growing.
– Luke Caputo, 12/4/2020
We hope these recovery stories show how other survivors were affected by a stroke in the brain stem and how intensive rehabilitation leads to recovery. Every survivor will experience a different journey, but it’s important to stay consistent with your rehab exercises. Believing that recovery is possible can motivate you to take action and continue working toward your unique goals.
Persevering on the Road to Recovery
The brain stem is responsible for many of the body’s vital functions. Therefore, a stroke in this area of the brain can be accompanied by severe secondary effects. Some of these effects include difficulty breathing, weakness, altered consciousness, and dysphagia.
Thankfully, the brain’s resilience and ability to heal can allow survivors to regain lost function. Through intensive rehabilitation, survivors like Becky and Luke can make remarkable recoveries. This requires consistency, dedication, and the motivation to keep working toward your goals.
We hope this article helped illustrate how a stroke can affect the brain stem and what to expect on the road to recovery. Every journey will look different, but many survivors can increase their function and independence through dedicated rehab.