A stroke is medical emergency that impacts the supply of blood in the brain. With appropriate and timely medical treatment, the individual’s life is often saved. However, any brain damage sustained will likely result in stroke side effects – more accurately referred to as secondary effects of stroke.
Every stroke is different and, as a result, every survivor will experience secondary effects differently. Being aware of the potential effects of stroke can help individuals and their families have an idea of what to expect as survivors begin their recovery process.
There are numerous secondary effects of stroke, ranging from physical impairments and sensory problems to cognitive deficits and emotional changes. This article was designed to offer a comprehensive overview of the most common effects of stroke. Use the links below to jump directly to any section.
- Why Do Secondary Effects of Stroke Occur?
- Physical Effects
- Cognitive Effects
- Behavioral/Emotional Effects
- Sensory/Perceptual Effects
- Medical Complications
Why Do Secondary Effects of Stroke Occur?
A stroke occurs when the supply of blood in the brain is compromised, depriving local brain tissue of oxygen-rich blood. While emergency medical treatments can help restore normal blood flow, the areas of the brain that were deprived of blood and nutrients during the stroke may sustain lasting damage.
Following a stroke, functions that were previously controlled by affected areas of the brain may be impaired or lost. These affected functions are referred to as the secondary effects of stroke.
The effects of stroke vary widely in type and severity, influenced by the size and locationof the stroke. Mild stroke survivors often experience minimal effects that resolve quickly, while survivors of massive stroke may sustain severe, long-lasting effects, such as paralysis. The types of effects that develop after stroke depend on the functions that affected areas of the brain were responsible for.
Although the size and location of a stroke can give individuals an idea of what effects they may experience, every stroke is different and every brain is wired a bit differently. During the stroke recovery process, repetitive and task-specific practice of affected skills can promote neuroplasticity, allowing adaptive rewiring of the brain to take place. This can allow healthy areas of the brain to assume control over functions that were previously housed in damaged areas.
Understanding some of the most common secondary effects of stroke can help survivors and their family members prepare for the road to recovery ahead. The following sections outline the many different effects of stroke and their potential treatments.
Physical Effects of Stroke
The most outwardly apparent effects of a stroke are those that impact the ability to move effectively. When a stroke affects an individual’s physical abilities, they may not be able to safely and independently accomplish their activities of daily living, such as eating, dressing, toileting, and moving throughout the home. The physical effects of stroke may also impact the ability to work, drive, cook, and participate in leisure activities.
Therefore, survivors and therapists alike are often highly motivated to address the physical effects of stroke. Below are some of the most common physical effects that stroke survivors may experience:
Hemiparesis or Hemiplegia
Motor impairments that affect one side of the body, usually opposite of where the stroke occurred, are commonly seen after stroke. Hemiparesis (one-sided weakness) and hemiplegia (one-sided paralysis) may be caused by a stroke in areas of the brain related to movement, such as the motor cortex.
Treatment involves physical and occupational therapy to rewire the brain, restore movement, and explore compensatory techniques as needed. Speech therapy may also be needed to address speaking and eating challenges if one side of the face has been affected.
Learn more about hemiparesis and hemiplegia after stroke »
Learned Nonuse
Often caused by over-relying on the unaffected side of the body, learned nonuse occurs when the affected muscles are not moved on a regular basis (either through active exercise or passive range of motion). This causes the affected muscles to gradually deteriorate until any function that was left intact following the stroke is also lost.
Learn how to prevent learned nonuse »
Changes in Muscle Tone
A stroke may result in changes in muscle tone. Flaccidity refers to soft, limp muscles, while spasticity refers to stiff, tight muscles. When spasticity is left unmanaged, it can progress into contractures, which are characterized by extreme muscle stiffness. Often seen in the toes and hands, contractures are caused by the shortening of the muscles or connective tissues that span one or more joints.
Treatment for changes in muscle tone often involve physical and occupational therapy. Survivors with contractures may use splints, braces or casts, passive and prolonged stretching exercises, or potentially surgery to manage their condition.
Learn more about flaccidity after stroke »
Learn more about addressing spasticity »
Balance Issues
Changes in the muscular system following stroke may result in poor balance, putting stroke survivors at risk of falling. If survivors also experience dizziness or vertigo after stroke, this risk may be compounded.
Rehabilitative exercises, particularly for the legs, feet, and core, can help restore strength and movement in the body and improve balance. In the meantime, a physical therapist can recommend an appropriate assistive device to improve safety, such as a cane or walker.
Learn more about improving balance after stroke »
Shoulder Complications
Because the shoulder joint can move in so many different ways, it is particularly vulnerable to injury. Many stroke survivors experience shoulder weakness and pain. If left untreated, more serious conditions may develop, such as shoulder subluxation (where the shoulder becomes partially dislocated) and frozen shoulder (where the surrounding ligaments become inflamed and tighten).
Learn more about shoulder pain after stroke »
Foot Drop
Characterized by difficulty with dorsiflexion (lifting the front part of the foot up towards the shin), foot drop is a condition that can make walking after stroke challenging. Treatment involves rehabilitative exercise and physical therapy, although wearing an AFO brace to prop the foot up and improve safety is often recommended while recovering.
Learn more about foot drop after stroke »
Dysphagia (Difficulty Swallowing)
Individuals who have difficulty swallowing after stroke likely are experiencing a secondary effect known as dysphagia. Survivors with dysphagia can work with speech language pathologists (SLPs) to retrain the brain to control the swallowing muscles. In rare cases, a feeding tube may be required.
Post-Stroke Fatigue / Excessive Sleeping
Fatigue after stroke is common, as the brain requires extra energy while healing throughout the recovery process. Everyday tasks may take more energy to complete, resulting in daytime sleepiness or fatigue. As a result, many survivors experience excessive sleeping.
Excessive sleeping early in the recovery process is often encouraged and beneficial. However, if this persists past the initial recovery stages, it may impede rehabilitation and be a sign of other underlying issues that should be addressed with one’s medical team.
Learn more about fatigue after stroke »
Physical and occupational therapy often focus on restoring physical abilities. Through consistent and repetitive practice, survivors may be able to rewire their brains and improve physical functions that were impaired or lost after stroke.
Cognitive Effects of Stroke
While not as outwardly apparent, the cognitive effects of stroke are important to understand. Changes in cognition can impair the ability to perform activities of daily living, communicate effectively with others, and manage work and/or household duties.
Cognitive changes are likely to occur after a frontal lobe stroke, since it is responsible for many of the higher-level cognitive functions. Here are a few of the most common cognitiveeffects of stroke:
Impaired Memory and Attention
The frontal lobe handles higher cognitive skills, such as memory and attention. When it sustains damage after stroke, executing everyday cognitive functions can become difficult.
Sometimes impaired attention and memory skills can improve on their own (spontaneous recovery). Other times, cognitive training with a speech or occupational therapist can promote improvements.
Learn more about cognitive training activities for stroke survivors »
Aphasia (Difficulty with Language)
The ability to produce and comprehend language are also considered cognitive skills. When one or both of these skills are impaired, an individual may have aphasia. Of note, aphasia is not caused by motor impairments in the mouth and tongue, but rather occurs when the brain has trouble finding words and/or connecting meaning to them. Aphasia commonly occurs following left hemisphere strokes, since the primary language centers of the brain usually reside there.
Speech therapy can address both expressive and receptive aphasia. If the survivor cannot talk at all, singing therapy may help. Alternative forms of communication can also be introduced during speech therapy, if needed.
Learn more about language problems after stroke »
Vascular Dementia
Post-stroke dementia, which can be referred to as vascular dementia, can stem from the impact of a stroke. Vascular dementia can cause cognitive issues, like impaired thinking and reasoning, memory loss, confusion, decreased attention, and more. It is important to work with one’s medical team for diagnosis and treatment.
Learn more about post stroke dementia »
Individuals experiencing the cognitive effects of a stroke are often recommended to work with speech language pathologists, also known as speech therapists. These professionals are highly skilled in working with stroke survivors with language difficulties and other cognitive issues.
Behavioral and Emotional Effects of Stroke
In addition to psychological impact of simply learning to live with any post-stroke impairments, the brain damage sustained during a stroke can cause emotional and behavioral changes. These changes may be challenging for survivors and their families to navigate, but behaviors and emotions are often able to be regulated with appropriate support.
Here are a few potential behavioral and emotional effects of stroke:
Depression and Anxiety
Depression and anxiety are among the most common secondary effects of stroke, with each affecting approximately one-quarter of all survivors. Treatments, including psychotherapy and medications, can help survivors maintain the motivation necessary to keep pursuing rehabilitation.
Learn more about depression after stroke »
Learn more about anxiety after stroke »
Pseudobulbar Affect
A post-stroke condition known as pseudobulbar affect, or emotional lability, can cause mood swings as well as random and inappropriate outbursts of laughter and/or crying. Treatment includes medication and/or psychotherapeutic intervention.
Learn more about pseudobulbar affect after stroke »
Behavioral Changes
Some stroke survivors demonstrate different behaviors after a stroke, such as anger or aggression. Sometimes irregular behaviors may occur, which could be a secondary effect caused by vascular dementia or other cognitive changes.
Learn more about behavior changes after stroke »
Treating and managing emotional and behavioral changes after stroke may involve various psychological therapies and/or medications. Support groups may also be vital sources of encouragement for both survivors and their family members.
Sensory and Perceptual Effects of Stroke
The thalamus and parietal lobe are two areas of the brain that play large roles in processing and regulating sensory input. Therefore, individuals who have had a stroke in these areas of the brain are likely to experience sensory and/or perceptual changes.
Here are some of the most common sensory and perceptualeffects of stroke:
Numbness and Tingling
Post-stroke numbness is a common secondary effect that causes a loss of sensation in the affected area. Some individuals may experience a total loss of sensation, while others may feel a tingling or pins-and-needles sensation.
Although some survivors experience spontaneous recovery of sensation, sensory reeducation is often recommended to help stimulate the brain to improve sensation. Of note, sometimes pins-and-needles sensations may occur before the onset of a more serious condition known as central pain syndrome.
Learn more about numbness after stroke »
Learn more about tingling sensations after stroke »
Pain
There are a number of reasons a survivor may experience pain after stroke. Sometimes localized pain can occur after a stroke, usually stemming from other effects like spasticity or contractures. This type of pain is best treated by addressing the underlying conditions. On the other hand, some conditions, such as central pain syndrome, may involve chronic pain.
Central post-stroke pain syndrome is a chronic condition that can occur months or even years after a stroke. Often seen after a thalamic stroke, central post-stroke pain syndrome may start with extreme sensitivity or pins-and-needles sensations before progressing into chronic pain. With the help of one’s medical team, survivors can learn more about what is causing their pain and how to address it.
Learn more about post stroke pain »
Visual Disturbances
When a stroke affects the brain’s visual processing abilities, vision may be affected. Some survivors develop double vision or sustain visual “field cuts” where half (or sometimes a quadrant) of the visual field is missing. Unlike some of the other sensory effects of stroke, vision problems commonly occur after an occipital lobe stroke. Treatment may include vision training and/or specialized glasses.
Learn more about regaining vision after stroke »
Hemineglect
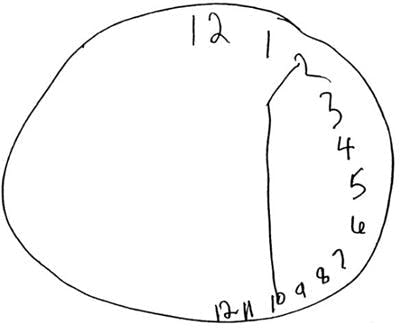
Image from Journal of Neurology
Hemineglect is a spatial awareness problem that prevents survivors from noticing half of their environment and body — often on their left side (informally known as left neglect). If someone with left neglect is asked to fill in the numbers on an empty clock, they may cram everything into the right side without realizing it, as shown in the image above. Treatment may involve visual scanning tactics or intentionally bringing awareness to the affected side.
Learn more about hemineglect »
The sensory and perceptual effects of stroke vary widely. Depending on which effects are experienced, individuals may work with a number of medical professionals to address these deficits, including occupational therapists, neurologists, neuro-ophthalmologists, and/or pain specialists.
Medical Complications After Stroke
Because of the impact a stroke can have on the brain and body, survivors may experience medical complications. Some are primary complications arising as a direct result of stroke, while others are secondary complications caused by the effects of stroke.
Here are some of the most common medical complications that may occur after stroke:
Bedsores
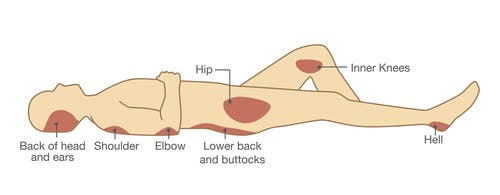
Bedsores, also known as pressure ulcers, may develop when there is prolonged pressure on certain areas of the body due to decreased mobility. Pressure ulcers often develop during longer hospital stays and in those who are unable to get out of bed. Although they are unfortunately very common among stroke survivors, bedsores can be prevented by re-positioning the body every few hours.
Learn more about recovery when bedridden after stroke »
Incontinence
A stroke can affect the ability to control the bladder and/or bowel movements, a condition known as incontinence. It can vary in severity, causing difficulties such as light leaking or complete loss of control. Bowel and/or bladder retraining programs may help address incontinence.
Learn more about incontinence after stroke »
Seizures
About 7% of survivors experience seizures after stroke. Seizures occur when there is sudden disorganized electrical activity in the brain, causing changes in movement (e.g. convulsions), behaviors, and levels of awareness or sensation. If seizures occur more than once, the individual may be diagnosed with epilepsy. Common treatments include anticonvulsant medication or a vagus nerve stimulator.
Learn more about seizures after stroke »
Pneumonia
Sometimes stroke survivors with dysphagia (impaired swallowing) accidentally inhale food into the lungs. These occurrences are known as aspirations, which can lead to pneumonia in stroke survivors. Pneumonia should be taken very seriously because it is one of the leading causes of mortality after stroke.
Learn more about pneumonia after stroke »
Deep Vein Thrombosis (DVT)
Deep vein thrombosis is a medical condition where blood clots form in veins of the legs, often due to impaired mobility. Since many stroke survivors struggle with mobility issues, they may be at increased risk of DVT during recovery. Individuals at risk of developing a DVT may be prescribed blood-thinning medication as a preventative measure.
Learn more about DVT after stroke »
Headaches
Headaches following a stroke are a common and worrisome event. If a survivor experiences severe or mild headaches that last for longer than a few hours, seek medical attention immediately because it may signify further medical complications.
Learn more about headaches after stroke »
Seek medical attention if any of these effects or complications are present after a stroke. A medical evaluation is the best way to determine if new effects require further treatment.
Understanding the Effects of Stroke
A stroke may cause a wide variety of secondary effects. Depending on the location and the size of the stroke, some effects may resolve quickly, while others may last for several months or years.
Through rehabilitation, many individuals are able to recover from the secondary effects of stroke. Even if the stroke occurred months or even years ago, there is always hope for recovery.