Damage to Wernicke’s area, located in the left hemisphere of the brain, can lead to various speech and language disorders, particularly Wernicke’s aphasia. Individuals with Wernicke’s aphasia can typically speak fluently, but their speech is often nonsensical and lacks meaning.
This condition can make it difficult for the survivors to communicate with their loved ones, which can be frustrating. Fortunately, Wernicke’s aphasia can be improved with a combination of speech and language therapy exercises and helpful tactics.
This article will discuss what happens when Wernicke’s area sustains damage and how the recovery process works.
Use the jump links below to navigate through the article:
- What is Wernicke’s area?
- Causes of damage to Wernicke’s area
- Symptoms of Wernicke’s aphasia
- How to recognize Wernicke’s aphasia
- Stages of recovery
- How to treat damage to Wernicke’s area
What is Wernicke’s Area?
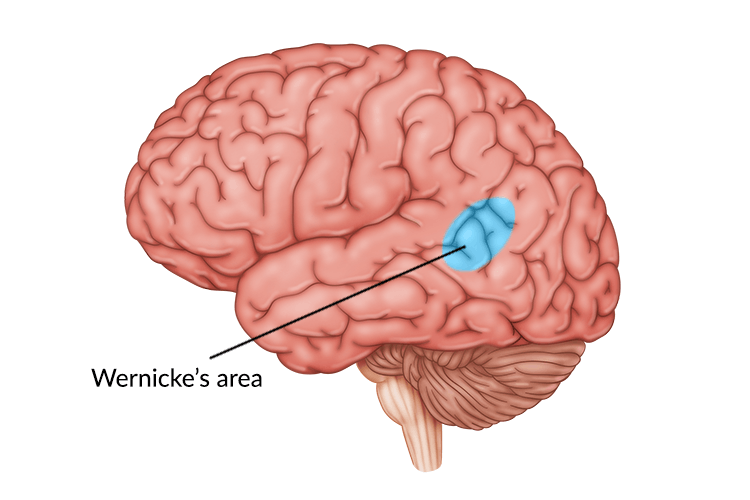
Wernicke’s area is located in the posterior part of the left hemisphere of the brain. It was first discovered by a neuropsychiatrist named Carl Wernicke who studied the effects of brain damage on individuals with communication disorders such as aphasia.
Aphasia is a language and speech disorder that can make it difficult to understand or produce words. Wernicke discovered that some survivors were able to speak but could not form coherent sentences. He found that these survivors would also use random words without realizing it, making it difficult to communicate effectively.
Through further research, Wernicke discovered that individuals with this type of aphasia had lesions in the left hemisphere of the brain, specifically near the back of the temporal lobe. This region of the brain, now known as Wernicke’s area, is primarily responsible for the comprehension of written and spoken language.
Causes of Damage to Wernicke’s Area
Damage to Wernicke’s area can be caused by traumatic brain injury, stroke, brain tumors, infectious diseases, and other neurological disorders.
The most common cause of damage to Wernicke’s area is ischemic stroke. While there are many types of aphasia, studies show that between 25-40% of stroke survivors acquire one or more types of aphasia due to the areas of the brain that have been damaged.
Damage to Wernicke’s area most often results in fluent aphasia, also known as receptive aphasia or Wernicke’s aphasia. This type of aphasia makes it difficult to understand both spoken and written words. Speech-language pathologists (SLPs) can help survivors differentiate between symptoms of Wernicke’s aphasia and other speech and language disorders.
Symptoms of Wernicke’s Aphasia
Unlike more common types of aphasia, Wernicke’s aphasia does not affect a person’s ability to produce words. Rather, those with Wernicke’s aphasia have lost their ability to grasp the meaning of words. This results in their speech sounding like “word salad”, or words that have just been tossed together.
Symptoms of Wernicke’s aphasia may include:
- Producing sentences that lack meaning
- Difficulty repeating words or phrases
- Forming sentences with several random words
- Difficulty with reading and writing
- Trouble understanding others
Additionally, many survivors with Wernicke’s aphasia may not realize they have any problems with speech. As a result, they might express feelings of confusion or frustration when they are unable to communicate with their loved ones. Therefore, it helps to learn how to recognize symptoms of Wernicke’s aphasia and find effective management techniques.
Recognizing Wernicke’s Aphasia
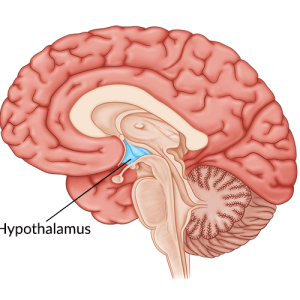
When damage is localized to Wernicke’s area, survivors often do not experience any other cognitive or physical impairments. This is because Wernicke’s area is located toward the back of the brain, away from many areas that are involved in higher level cognitive skills and motor abilities, such as the frontal lobe.
For this reason, individuals with Wernicke’s aphasia may still be able to walk and perform the activities of daily living on their own. However, since those with Wernicke’s aphasia are often relatively high-functioning, it may seem like survivors are not struggling with a speech or language disorder caused by a brain injury or stroke.
As a result, individuals may be overlooked and misdiagnosed. Sometimes others can even think those with Wernicke’s aphasia are intoxicated due to their jumbled speech patterns. Adding to these challenges, survivors often find it difficult to communicate their feelings and symptoms to their loved ones.
Therefore, understanding and recognizing the symptoms of Wernicke’s aphasia is especially important in order to advocate for an accurate diagnosis and treatment plan.
Fortunately, speech-language pathologists (SLP) can recognize Wernicke’s aphasia and provide survivors and their loved ones with strategies to manage daily life. They can also provide a rehabilitation plan tailored to the survivor’s specific needs.
Stages of Recovery from Wernicke’s Aphasia
Recovery may look different for every survivor depending on the cause of aphasia and the severity. However, there are several stages that many individuals go through when recovering from damage to Wernicke’s area.
Stages of recovery from Wernicke’s aphasia may include:
- Stage 1: During the initial stage of Wernicke’s aphasia, survivors may feel confused and may have minimal understanding of written or spoken words.
- Stage 2: In the second stage, confusion may decrease but speech may still not be clear. As a result, individuals may express feelings of frustration when others cannot understand them.
- Stage 3: Survivors may now understand words in highly contextual settings, such as being asked simple questions like “do you want a bowl or a plate?”.
- Stage 4: Speech may have a normal rhythm and intonation, but words may still lack meaning. However, comprehension of words may have improved.
- Stage 5: Individuals may begin to become more self-aware, realizing that their words do not make sense and striving to form better sentences.
- Stage 6: Survivors may be able to echo spoken words and read single words or simple phrases.
- Stage 7: At this stage, individuals may be able to use appropriate words based on the context and form better sentences. They may still struggle with word finding at times, referred to as anomic aphasia.
Every brain heals at a different pace and therefore these stages may not be accurate for every survivor. Nonetheless, understanding these stages can help reduce feelings of stress and frustration for survivors and their loved ones.
How to Treat Damage to Wernicke’s Area
An SLP can provide survivors with effective management techniques to help improve communication skills affected by Wernicke’s aphasia. This can include a combination of speech and language exercises both at a clinic and at home.
Some helpful tactics individuals can use to communicate better include:
- Using gestures
- Drawing pictures
- Writing down important information
- Slowing down your speech to give others time to process
- Talking about things and asking contextually relevant questions
While using these tactics is helpful during recovery, it may still take time and patience for survivors to effectively communicate with loved ones. However, it’s important to remember that having Wernicke’s aphasia does not equal loss of intelligence. The brain is healing, and it may take time, but there is hope for recovery.
Working with a speech language pathologist can be beneficial at any stage of recovery. However, most improvements after a neurological injury occur in the first few months.
Following an injury to the brain, such as a traumatic brain injury or stroke, the brain enters a heightened level of neuroplasticity. Neuroplasticity refers to the brain’s ability to rewire and repair itself. This allows great improvements to occur during the initial recovery period.
However, engaging in high repetition exercises can boost neuroplasticity at any point of recovery. Consider working with an SLP to learn customized speech and language exercises, and ask for a home exercise program in order to optimize improvements through neuroplasticity.
Understanding Damage to Wernicke’s Area
Damage to Wernicke’s area can lead to disorders associated with speech and language such as Wernicke’s aphasia. This condition causes difficulty with understanding language and forming meaningful sentences.
Wernicke’s aphasia can make it difficult to communicate effectively, which can be frustrating for both the survivor and their loved ones. Fortunately, SLPs can provide individuals with therapeutic exercises and tactics to help improve communication skills caused by damage to Wernicke’s area.
We hope this article helped you understand the effects of damage to Wernicke’s area and how to improve communication.