Spastic cerebral palsy (CP) is the most common type of cerebral palsy, making up about 80% of all cases. Despite being so prevalent, each individual experiences this type of CP differently and will benefit most from a personalized approach to management.
To help you understand what to expect if your child has spastic cerebral palsy, this article will cover the different types, causes, signs and symptoms, as well as management – let’s dive in!
Jump to a section
- Causes of Spastic Cerebral Palsy
- Signs and Symptoms
- Types of Spastic Cerebral Palsy
- Management of Spastic Cerebral Palsy
Causes of Spastic Cerebral Palsy
As with all forms of cerebral palsy, spastic cerebral palsy is caused by damage to the developing brain before, during, or shortly after birth. Specifically, it’s caused by damage to the motor cortex, which is the part of the brain primarily responsible for controlling voluntary movement.
Common causes of spastic CP include:
- Premature birth
- Infection
- Lack of oxygen in the brain
- Stroke
- Genetic factors
- Head injuries
- Cerebrovascular accidents
Depending on the severity of the damage to the brain, motor impairments may range from mild to severe. In the following section, we’ll explain common symptoms of spastic cerebral palsy.
Signs and Symptoms of Spastic Cerebral Palsy
As its name suggests, spastic cerebral palsy is mostly characterized by spasticity (involuntary muscle contractions). Spasticity occurs because damage to the brain disrupts the transmission of signals to the muscles.
The sensory and motor fibers within the central nervous system work together to regulate the tightening and relaxing of muscles. Damage to the brain or spinal cord can disrupt this system and cause muscles to involuntarily contract.
Spasticity is the underlying cause of many secondary complications of spastic CP, including:
- Abnormal gait
- Stiff movements
- Difficulties with balance
- Slow movements
- Chronic pain
- Clenching of the fingers or toes
- Spasms or jerky movements
- Chewing, swallowing, or speaking difficulties
- Developmental delays
Additionally, spastic cerebral palsy may only affect certain areas of the body. For example, depending on the severity of damage to the brain, individuals with spastic CP may only be affected on one side of the body or a single limb. Up next, we’ll review the various types of spastic CP and how they affect the body.
Types of Spastic Cerebral Palsy
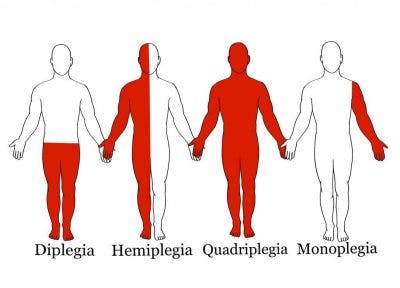
While spastic cerebral palsy is the most common type of CP, it can be further categorized by which areas of the body it affects. Generally, the more severe the brain damage is, the more areas of the body will be affected.
The various types of spastic CP are:
- Spastic hemiplegia: motor impairments in one side of the body
- Spastic monoplegia: motor impairments in one limb (usually an arm)
- Spastic diplegia: motor impairments in both legs (may also mildly affect the arms)
- Spastic triplegia: motor impairments in 3 limbs (typically both legs and an arm)
- Spastic quadriplegia: motor impairments that affect all four limbs (may also affect the muscles around the mouth)
Spastic hemiplegia, diplegia, and quadriplegia are most common, while spastic monoplegia and triplegia are more rare.
Regardless, management for any type of spastic CP involves minimizing the progression of spasticity to optimize overall mobility and quality of life. Now that you understand the cause, symptoms, and types of spastic CP, let’s explore effective ways to manage the condition.
Management of Spastic Cerebral Palsy
To effectively manage spastic cerebral palsy and improve motor functions, individuals should focus on promoting neuroplasticity. Neuroplasticity is the brain’s ability to rewire itself. While damaged parts of the brain cannot heal, affected functions may be reassigned to healthy areas of the brain through consistent stimulation.
The more repetitions a person performs, the stronger the neural pathways for that function become.
It is ideal to start management as early as possible because children’s brains have higher levels of plasticity than those of adults. As a result, it is usually easier for children to acquire new skills to replace abnormal movement patterns.
Below, we’ll provide some of the most effective ways to manage spastic cerebral palsy.
1. Physical Therapy

Physical therapy for spastic cerebral palsy focuses on improving an individual’s mobility through targeted exercises.
By continuously stimulating the muscles and moving the joints, individuals with spastic CP may expand their range of motion, improve circulation, and promote neuroplasticity to reduce spasticity.
2. Occupational Therapy
Occupational therapy involves improves one’s functional abilities, primarily through practicing activities of daily living such as brushing one’s teeth or getting dressed.
By practicing everyday activities, individuals with spastic CP develop the skills necessary to optimize their independence.
3. Orthotic Devices

Orthotic devices like braces, splints, and casts can be extremely helpful for managing spastic cerebral palsy.
While the brain damage that caused cerebral palsy will not progress, symptoms such as spasticity may increase. The more severe one’s spasticity becomes, the more difficult it becomes to move. Some individuals with cerebral palsy lose the ability to walk as they get older due to increasing spasticity.
Orthotic devices promote proper form and musculoskeletal alignment. They’ll also mildly stretch spastic muscles and support underused muscles.
4. Botox
Botox is a nerve blocker that is directly injected into spastic muscles to relieve high muscle tone.
However, it’s important to understand that Botox is only a temporary spasticity treatment and its effects typically last between 3-6 months. To promote long-term spasticity relief, individuals should take advantage of the effects of Botox and pursue intensive physical therapy to promote neuroplasticity.
5. Muscle Relaxants
Baclofen is a muscle relaxant that reduces spasticity by regulating the release of neurotransmitters that cause muscle contractions.
Like Botox, the effects of muscle relaxants are temporary and may not be ideal for long-term use. Generally, muscle relaxants do not last very long and will need to be administered more regularly than Botox.
6. Speech Therapy
Individuals with motor impairments involving the mouth will benefit from speech therapy. A speech-language pathologist guides your child through exercises to strengthen their oral motor muscles and improve their ability to eat and speak.
Speech therapy may also help children who are non-verbal learn how to use augmentative and alternative communication devices such as communication boards or voice generators to improve communication with others.
7. Surgery
Surgery for spastic CP is generally only recommended if other methods of management prove ineffective. The most common surgery for spastic cerebral palsy is selective dorsal rhizotomy. It involves severing nerve roots at the spinal cord to relieve severely spastic muscles.
Other commonly performed surgeries for spastic CP include muscle and tendon lengthening surgeries as well as baclofen pump implantation.
Understanding Spastic Cerebral Palsy: Key Points
Although spastic cerebral palsy makes up approximately 80% of all cerebral palsy cases, everyone experiences it differently. As a result, management for cerebral palsy should be personalized to each individual’s unique symptoms.
While cerebral palsy is a life-long condition, individuals with spastic CP may enhance their mobility by promoting neuroplasticity. With continuous practice and spasticity management, movement patterns may be improved.
We hope this article helped you better understand what spastic CP is and how to manage it.