Tremors after brain injury, also known as post-traumatic tremors, are a rare side effect of TBI. They mostly occur after damage to the cerebellum. Sometimes, however, other movement disorders can cause symptoms that look like tremors but are in fact something else.
Tremors are involuntary muscle contractions that create shaking movements in the head or other parts of the body such as the arms, legs, torso, and vocal chords. It can occur intermittently or be constant. Though it is often not a life threatening condition, it can be uncomfortable and disabling at times, interfering with daily activities.
Fortunately, there are various treatment options available, depending on the type and severity of the post-traumatic tremor. Obtaining a proper diagnosis is essential. This article will discuss the possible causes of tremors after head injury, symptoms, and effective management techniques.
What Causes Post-Traumatic Tremors?
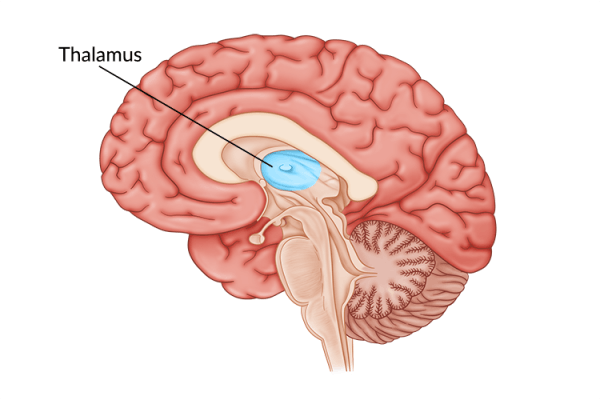
Generally, post-traumatic tremors occur from damage to the areas of the brain responsible for motor control such as the cerebral cortex, frontal lobe, thalamus, basal ganglia, or cerebellum. Aside from a traumatic brain injury, tremors can occur sporadically (on their own) or be a result of another neurological disorder including multiple sclerosis, stroke, or neurodegenerative diseases like Parkinson’s disease.
However, sometimes non-neurological disorders contribute to the development of tremors such as:
- Overactive thyroid
- Mercury poisoning
- Kidney or liver failure
- Alcohol abuse or withdrawals
- Anxiety and/or panic
Tremors may also be a side effect of asthma medication or other such as amphetamines, corticosteroids, psychiatric drugs, and even caffeine. Therefore, it’s important to consult with your doctor to obtain a proper diagnosis for post-traumatic tremors.
What Are the Symptoms of a Post-Traumatic Tremor?
Shaking after head injury is one of the biggest signs of a post-traumatic tremor. It can occur in one or more areas of the body such as the hands, arms, legs, head, and torso. Tremors can also be accompanied by other symptoms, including:
- Trembling or shaky voice
- Difficulty holding objects steadily like utensils
- Difficulty writing and/or drawing
Tremors after head injury can become triggered or exacerbated with physical exhaustion, strong emotions such as stress, and with certain postures or movements. To manage these symptoms, it can help to be aware of your triggers and surroundings.
Types of Tremors After Head Injury

Tremors are a TBI side effect with one of the longest onset delays, usually appearing several months or years after a brain injury. As such, it’s crucial to consult with your doctor or therapist if you notice any new or recurring symptoms months or even years after a brain injury.
Tremors are classified into two main categories, resting tremor or action tremor.
- Resting tremors occur when the muscles are relaxed, often only affecting the hands and fingers. For example, individuals sitting down with their hands placed on their lap may feel shaking in their hands or legs even at rest. Resting tremors are seen in many individuals with Parkinson’s disease.
- Action tremors occur during voluntary movement of a muscle such as when an individual moves or performs a complex task. For example, when an individual is writing or holding a heavy object in the same position, their hands may begin to shake and worsen over a longer period of performing that action.
Action tremors are more common than resting tremors, which are usually classified by their appearance and origin. While there are over 20 different types of tremors, this article will focus on the most common types of tremors that occur after brain injury, which include:
- Essential tremors are one of the most common types of tremors after head injury that occur primarily in the hands and arms. They can affect the voice box, causing quivering in the voice. They are also known as familial tremors because they are thought to be caused by a genetic risk factor. However, stress, exhaustion, and low blood pressure can trigger and increase the severity of essential tremors after head injury.
- Dystonic tremors occur in individuals with dystonia after brain injury, a common movement disorder where incorrect signals from the brain cause the muscles to overreact. It can affect the hands, arms, and head and usually result in abnormal postures due to forceful spasms/cramps or unwanted movements.
- Cerebellar tremors commonly occur after injury to the cerebellum. They create slow, visible shaking movement in the arms and legs. Cerebellar tremors occur at the end of purposeful movements such as pushing a button.
- Midbrain tremors, also known as rubral tremors, result from damage to the neural pathways connecting the cerebellum to the brain stem. Midbrain tremors are usually present during voluntary maintenance of posture, such as when the arms are stretched out. The midbrain also contains the substantia nigra and damage to this area can lead to parkinsonian tremors.
- Parkinsonian tremors are a common symptom of Parkinson’s disease. It can include shaking in one or both hands at rest, as well as the chin, lips, face, and legs. Parkinsonian tremors can appear in just one limb or one side of the body, and progress to both sides depending on the severity. It is often increased by stress and other strong emotions. Studies estimate that Parkinsonism may be a consequence of up to 1.5% of all traumatic brain injuries.
- Psychogenic tremors, also known as functional tremors, can be caused by underlying psychological conditions such as depression or post-traumatic stress disorder (PTSD), both of which can occur after brain injury. Symptoms vary but can often be abrupt and affect multiple body parts. It increases during stress-related circumstances, and can decrease when distracted or calm
There are numerous types of tremors that can occur after a head injury. While your doctor will make an assessment and proper diagnosis, it helps to know what signs to look for and how to differentiate tremors from other movement disorders.
Other Movement Disorders That Cause Shaking After Head Injury

While shaking after a head injury can be diagnosed as a tremor, it can often be confused with other involuntary movement disorders such as clonus or muscle spasms. Since treatment depends on the diagnosis, it’s important to distinguish tremors from other related conditions.
Muscle spasms occur when the muscle contracts involuntarily, but the rate at which it contracts can vary and be random; whereas a tremor usually has a rhythmic pattern of movements. Tremors are also painless, but muscle spasms can cause contortions and be accompanied by extreme pain. Rhythm and pain are two key differentiating symptoms to look for if you are experiencing uncontrolled muscle movements.
Clonus is another movement pattern commonly mistaken for tremors because of its similar symptoms including: rhythmic shaking, pain free, and primarily present in the arms and legs. However, with clonus one of the main distinguishing features is when stretching the muscles. When the affected limb is stretched out, it will trigger and even increase the shaking, opposite to tremors.
Diagnosing Post-Traumatic Tremors
To determine the cause and type of tremor you are experiencing after a head injury, a couple of tests will be performed. Doctors may first order an MRI, CT Scan, or another similar imaging exam to determine if the areas of the brain responsible for motor control have been affected.
The long delay between brain injury and tremor onset may sometimes make it challenging to determine whether brain damage directly caused the tremors. To rule out any physiological causes of tremors such as overactive thyroid or mercury poisoning, may also perform blood tests and any additional tests necessary.
With a proper diagnosis of movement disorders after a traumatic brain injury, treatment can begin. Let’s explore effective management techniques for post-traumatic tremors.
Treating Tremors After Brain Injury

Every brain injury is different and treatment for tremors after brain injury will also vary depending on the type of diagnosis and severity. Sometimes the more severe a tremor, the more invasive the treatment. Therefore it’s important to speak to your doctor about the best treatment options for your condition.
Here are some of the most effective treatments for post-traumatic tremors:
Therapy
Therapy exercises help activate neuroplasticity, the brain’s ability to heal and rewire itself. After a brain injury, neural pathways used for communication between the brain and the rest of the body may become damaged or destroyed. Through neuroplasticity, existing neural pathways are strengthened and new ones are created. Thus, with better communication between the brain and body/muscles, the better motor control. Types of therapy may include:
- Physical therapy: focuses on building strength, improving muscle control, and restoring function through balance, coordination, and other types of physical exercises.
- Occupational therapy: focuses on teaching survivors new ways to perform daily activities, keeping survivors engaged in meaningful daily tasks, and therefore more active in general.
- Speech-language therapy: focuses on evaluating speech, language, communication, and swallowing disorders that can sometimes be impacted by tremors after brain injury.
In addition to performing therapeutic exercises, therapists may also recommend orthotic braces or weights to help reduce the effects of a tremor by maintaining stability in the affected muscles.
Medication
Along with therapy, there are several types of medication your doctor may prescribe to help treat post-traumatic tremors. This can include:
- Beta-blocking prescription drugs such as propranolol, atenolol, and sotalol can help treat essential tremors after a brain injury and a couple types of action tremors by blocking nerve impulses to the muscles.
- Tranquilizers, which are also known as benzodiazepines, may help relieve post-traumatic tremor symptoms. While tranquilizers such as clonazepam and alprazolam are usually effective, it is a less popular option due to unwanted side effects including sleepiness, lack of coordination, and poor concentration. Be cautious when taking these medications by having a caregiver or friend nearby.
- Anti-seizure medication, such as primidone, gabapentin, and topiramate, is usually given to individuals with essential tremors who don’t respond well to beta-blockers. However, tremors can be a result of certain medication including anti-seizure medication, therefore it is crucial not to take any new medication without consulting your doctor.
- Botulinum (botox) injections are one of the most effective ways to treat tremors after head injury, with long-lasting effects such as 3 months. However, it can often be accompanied by weakness in the hands and fingers. Consult with your doctor to see if injections are safe and suitable for you.
Prescribed medication can be helpful, and at times be necessary, depending on the severity of the post-traumatic tremor. While most are effective, they can leave unwanted side effects that can interfere with daily activities. If you are interested in taking medication make sure to consult with your doctor or specialist first.
Surgery
When therapy and medication are not providing positive results, doctors may recommend surgical intervention. These treatment options are more invasive and should be explored once all other options have been exhausted.
Surgical options for post-traumatic tremors may include:
- Deep brain stimulation (DBS) is an FDA approved mechanism for post-traumatic tremors that involves surgically implanting electrodes to send high-frequency signals to the thalamus (a structure in the brain that controls involuntary movements). This helps reduce tremors including essential, parkinsonian, and dystonic tremors. Although highly invasive, studies have shown promising results. Possible side effects include dysarthria (slurred speech) and imbalance.
- Thalamotomy is an invasive surgical procedure that involves the destruction of a tiny area in the thalamus through radiofrequency ablation that may be contributing to tremors. It is usually performed on one side of the brain opposite from the tremor. Surgery on both sides is not recommended due to the effects it can cause such as problems with speech.
When tremors after head injury are severe, surgery may sometimes be an option. However, surgical interventions are invasive and can lead to unwanted side effects or complications. Ask your doctor if surgery is an appropriate option for your condition.
Lifestyle Changes
While tremors after head injury are usually caused by damage to the areas of the brain that control movement, there are various contributing factors that can exacerbate them including stress, anxiety, and certain substances.
Adapting new lifestyle changes such as reducing stress and caffeine-intake can help reduce post-traumatic tremor symptoms. For instance, to help manage stress and anxiety, you can try behavioral relaxation training, which focuses on labeling feelings and defusing them with the help of a therapist. With stress levels under control, tremors may improve.
Overcoming Body Shaking After Head Injury
Body shaking after head injury can occur after damage to the areas of the brain responsible for motor control. Because post-traumatic tremors usually have a delayed onset, it’s important to learn how to recognize the signs and symptoms and how to differentiate them from other conditions.
Obtaining a proper diagnosis is essential to receive proper treatment. There are various management techniques available for tremors after head injury, just consult with your doctor to make sure they are safe and appropriate for you.
We hope this article helped you understand shaking after head injury and the possibilities of overcoming post-traumatic tremors.