No products in the cart.
No products in the cart.
No products in the cart.
No products in the cart.
Home » Neurological Recovery Blog » Spinal Cord Injury » Complications of Paraplegia: Why They Occur and How to Manage Them
Last updated on November 4, 2020

Complications of paraplegia can arise immediately after spinal cord injury, years later, or anytime in between.
Therefore, it’s essential to be aware of complications and understand what you can do to prevent them from worsening.
This article will go over 9 common complications of paraplegia and how to manage them.
The development of secondary complications after spinal cord injury can significantly affect rehabilitation outcomes and quality of life. Complications of paraplegia can affect energy levels, quality of sleep, mood, and motivation for recovery.
By minimizing the onset of complications through preventive measures, individuals can improve their recovery outcomes. Additionally, even if your spinal cord injury occurred years ago, you can still work on recovery. It’s never too late!
You’re about to learn about 9 common complications of paraplegia:

Spasticity refers to involuntary muscle contractions in areas below your level of injury. It occurs because SCI disrupts the communication between your brain and body.
As a result, your muscles become hypersensitive to stimuli. Additionally, because they do not receive signals from the brain to relax, they remain contracted for extended periods.
Poorly managed spasticity can lead to other complications of paraplegia such as contractures, pain, poor quality sleep, and difficulty with transferring or walking.
However, moderate spasticity can also be beneficial. For example, individuals with paraplegia can take advantage of increased tone in their leg to prop themselves up when performing transfers and standing.
One of the most common complications of paraplegia is muscle atrophy due to reduced physical activity.
Muscle atrophy is when your muscles shrink from disuse. Think ‘use it or lose it.’ Our bodies are constantly adapting based on our everyday actions and when you significantly reduce movement and weight-bearing in the legs, the muscles will shrink to preserve energy.
Low muscle mass can increase your risk of injury, cause blood to pool in your legs, and slow down your metabolic rate. Even if you have severe paraplegia, passive movement of your legs is essential to promote circulation, metabolism, and stimulate the spinal cord.

Another common complication of paraplegia is bowel and bladder dysfunction. After spinal cord injury, patients may be unable to feel when their bladders are full or when they need to empty their bowels.
Additionally, they may not be able to control the contracting or relaxing of their urethral or anal sphincters, so accidents or physical discomfort can occur.

Autonomic dysreflexia is a complication that can occur in individuals with T6 level spinal cord injuries and above. It describes the body’s hyperactive response to sensory stimuli due to disrupted communication between the brain and body.
The autonomic nervous system is responsible for involuntary body functions like temperature regulation, heart rate, and blood pressure. As a result, when areas below the level of injury are stimulated, individuals may experience:
Autonomic dysreflexia can be caused by extreme temperatures, skin irritations, tight clothes, and a full bladder. Therefore, it’s essential to be aware of your surroundings and avoid sitting or lying on something that can irritate the skin.
Individuals with paraplegia have an increased risk of developing pressure sores due to lack of movement.
Typically, people start to feel restless after sitting or lying in the same position for too long and will move around. However, due to loss of sensation following a spinal cord injury, many paraplegics may not feel the urge to move around.
Pressure sores are the result of prolonged pressure on the skin. Blood flow is cut off and tissues start to die, which makes the skin more susceptible to breakdown.
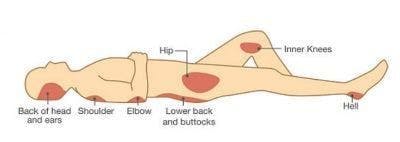
Pressure sores typically occur in areas of the body where the bones and skin are very close together like the elbows, shoulders, hips, knees, and ankles.

About 40-60% of all spinal cord injury patients develop neuropathic pain below their level of injury.
This type of pain is caused by damage to the nerves. Some people describe feeling pins and needles while others may feel burning or stabbing sensations.
People with paraplegia can also experience musculoskeletal pain above their level of injury from increased dependence of the arms. For example, you might overexert your arms when moving around in a wheelchair for too long.
Luckily, this type of pain is more bearable and can usually be relieved through rest.
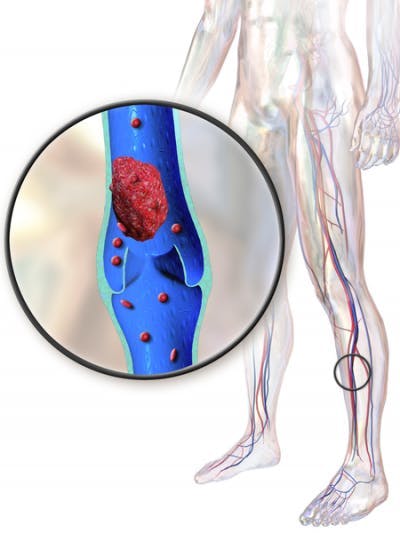
Deep vein thrombosis is a complication of paraplegia that occurs when a blood clot forms in the legs due to lack of movement. It can cause swelling, aching, and poor blood flow in the lower body.
Additionally, if part of the blood clot travels up to the lungs, it can cause a pulmonary embolism. Pulmonary embolisms occur when blood clots block arteries in the lungs, resulting in sudden breathing difficulties and chest pain.
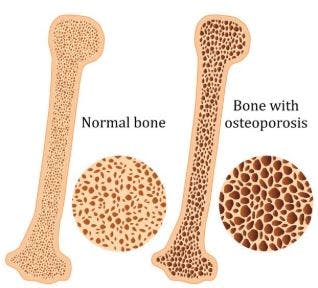
After a spinal cord injury, mobility becomes restricted, so many people can’t walk as much as they used to. Because the bones in the legs no longer bear as much weight, they lose bone mineral density below their level of injury.
Generally, the severity of injury is correlated to the severity of bone loss. Therefore, individuals with complete spinal cord injuries experience more severe osteoporosis than individuals with incomplete spinal cord injuries.
The effects of osteoporosis are most significant in the initial 12-18 months following a spinal cord injury. It’s suggested that on average, SCI patients experience bone loss at a rate of 4% per month.
While unmanaged osteoporosis will continue to progress for several years, it occurs at much a slower rate.

Because spinal cord injuries can require major changes to one’s lifestyle, the development of mental health complications like depression and anxiety extremely common. About 11-37% of SCI survivors experience depression and 15-32% experience anxiety.
Mental health disorders are caused by chemical imbalances in the brain. Both anxiety and depression can significantly affect your quality of life as they interfere with your motivation, energy levels, quality of sleep, and mood.
Now that you understand what these 9 complications of paraplegia are, let’s discuss what you can do to manage them.
Everyone experiences complications of paraplegia differently, so it’s essential to take a personalized approach to management. Generally, a combination of various management interventions proves the most effective, so you may need to go through some trial and error to find what works for you.
Below, we’ve listed some interventions that can help you manage complications of paraplegia:

By learning how to adapt and manage their complications, individuals with paraplegia can optimize both their physical and mental health.
Generally, those with more severe spinal cord injuries are more susceptible to complications; however, it’s always a good idea to be aware of problems that can arise and prepare for them.
Hopefully, this article helped you better understand the various complications that can result from paraplegia and how to manage them. Good luck!
Get instant access to our free exercise ebook for SCI survivors. If you liked this post, you’ll LOVE our emails and ebook.
Each exercise features pictures of a licensed therapist to help guide you. You’ll also receive our popular recovery emails with SCI survivor stories and other useful tips — you can opt out anytime.
We will never sell your email address, and we never spam.

Flint Rehab is the leading global provider of gamified neurorehab tools. Check out our bestselling tool by clicking the button below:
Depending on the severity of your spinal cord injury, there may be hope for improved mobility. Consistent at-home therapy is key to making this happen.
That’s why Flint Rehab created FitMi, a motion-sensing, gamified home recovery tool designed for neurological injury like SCI.
Here’s what others have said about it:
“I purchased this wonderful equipment for the use of spasticity for my right hand. Initially I wasn’t sure if it would work because of the various treatments I tried and also many physiotherapists who tried their level best, but didn’t achieve any positive results.
However after trying FitMi, I could feel that slowly and steadily I am improving. It’s really a great device that minutely takes care of each and every muscle of your affected body part. The biggest plus point is, you can use this device anywhere, anytime with precise exercises that you need and also saves your money and time spent on your physiotherapist.“
— Chandrakiran
FitMi works by encouraging you to practice rehab exercises with high repetition. On average, survivors complete hundreds of repetitions per half hour session.
“Massed practice” like this helps stimulate and rewire the nervous system. While you can achieve massed practice with a written sheet of exercises, it can be tough to stick with it consistently — and consistency is key to recovery.
FitMi helps transform rehab exercises into an engaging, interactive experience. The yellow and blue “pucks” track your movement and provide feedback. All of this comes together for a motivating home therapy program.
A survivor named Tom put it perfectly:
“I believe this device will help me concentrate on making the repetitive actions needed to obtain further movement range in my wrist and hand and arm and therefore rating it with five stars. My occupational therapist recommended to give this a try. I have been using FitMi for just a few weeks. I feel more at ease in flexing.”
If you’d like to learn more about FitMi, click the button below:
Do you have this 15 pages PDF of SCI rehab exercises?
Get a free copy of our ebook Rehab Exercises for Spinal Cord Injury Recovery. Click here to get instant access.
Grab a free rehab exercise ebook!
Sign up to receive a free PDF ebook with recovery exercises for stroke, traumatic brain injury, or spinal cord injury below: