Paraplegia describes paralysis of the lower limbs. It’s most commonly associated with spinal cord injuries but can also occur following a variety of other neurological conditions.
Depending on the severity of the paralysis, individuals may experience various long-term outcomes. For example, some individuals may be wheelchair-dependent while others won’t. Fortunately, there are effective ways to improve your functional independence in both mild and severe cases of paraplegia.
To help you understand paraplegia, this article will discuss its:
What Causes Paraplegia?
Paraplegia describes paralysis in the lower body that is typically caused by neurological damage.
Weakness or paralysis in both legs that does not affect the arms generally suggests an abnormality or damage to the spinal cord or peripheral nerves. The spinal cord and peripheral nerves play a major role in the transmission of messages between the brain and body. Signals from the brain travel down the spinal cord and branch out to the peripheral nerves to reach the muscles.
Therefore, when the spinal cord or peripheral nerves are damaged, motor signals (signals that activate movement) may not be able to reach the muscles. As a result, individuals experience paralysis in the affected area.
Depending on the level of spinal cord injury, individuals may experience paralysis in various regions of their bodies. Individuals with paraplegia generally have damage to the thoracic, lumbar, or sacral regions of the spinal cord. Additionally, those with thoracic spinal cord injuries experience weakness or paralysis in the muscles that make up their trunk.
Sources of nervous system damage that can cause paraplegia include:
- spinal cord injury
- spinal cord compression
- transverse myelitis
- spinal tumors
- concussion (including epidural hematomas)
- transverse myelitis
- lupus myelopathy
- metabolic disorders (Krabbe disease, argininemia, etc.)
- spinal infections
- familial spastic paraplegia (genetic factors)
- congenital malformations (syringomyelia, arachnoid cysts, etc.)
- cerebral palsy
- spina bifida
Additionally, paraplegia may be caused by damage to the brain. Often, individuals with paralysis in the legs due to brain damage also experience mild weakness in the arms. However, the weakness or paralysis in the legs is much more severe than in the arms.
The following section will discuss the effects of paraplegia and how they can impact your everyday life.
Signs and Symptoms of Paraplegia
Paralysis in the legs can affect a variety of functions that impact your everyday life. Depending on the severity of the paralysis and how much of the legs are affected, individuals may experience paraplegia in various ways.
Location of spinal cord injury matters because each level of the spinal cord innervates (supplies energy and information) to different muscles in order to facilitate movement. The higher the location of your injury, the more functions are affected. This occurs because signals from the brain cannot pass through damaged regions of the spinal cord. As a result, all functions below the level of injury cannot receive signals and become paralyzed.
Likewise, the severity of damage matters because it determines whether neural pathways in the spinal cord have been spared (unaffected by injury) and are able to transmit messages between the brain and areas below the level of injury. The existence of spared neural pathways accounts for why individuals with paraplegia may experience weakness in the legs rather than complete paralysis.
Many individuals with paraplegia also experience sensation changes in their lower extremities. This is because information from the affected parts of the body cannot be transmitted through damaged areas of the spinal cord back to the brain, just like information can’t be transmitted from the brain to the body. Again, the severity of sensation deficits also depends on the level and severity of the spinal cord injury.
Specific Features of Paraplegia
- difficulties with standing and walking
- abnormal walking patterns
- loss of bladder or bowel control
- poor sitting and/or standing balance
- tingling, numbness, and/or pain in the affected regions
- spasticity (involuntary muscle contractions)
- sexual dysfunction
- scoliosis or other postural abnormalities
- foot deformity
- inability to walk/ wheelchair dependence
- muscle atrophy
- loss of sensation
- exaggerated tendon reflexes
While paraplegia may limit a variety of functions that require use of the legs, individuals have the potential to regain a great deal of functional independence by learning to utilize their arms to compensate and adapt. The following section will discuss the recovery outlook for individuals with paraplegia.
Recovery Outlook for Paraplegia
The severity of a spinal cord injury significantly affects whether individuals with paraplegia may be able to recover mobility. One way to classify the severity of a spinal cord injury is to determine whether it is complete or incomplete.
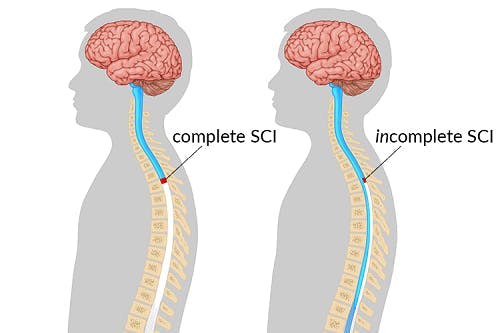
A complete spinal cord injury describes damage that transects all neural pathways at the level of injury. As a result, all connections between the brain and areas below the level of injury are cut off. Because damaged neurons are unable to regenerate, the effects of a complete spinal cord injury are permanent.
In contrast, an incomplete spinal cord injury describes partial damage to the spinal cord that results in spared neural pathways at the level of injury. Spared neural pathways play an essential role in determining whether recovery from paraplegia, including the ability to move and feel the lower extremities, is possible because they are capable of utilizing neuroplasticity.
Neuroplasticity is the central nervous system’s ability to make adaptive changes and reorganize its neural circuitry. It allows for functions affected by damage to be rewired to unaffected regions, strengthened, and improved. The most effective way to promote neuroplasticity is through highly repetitive, task-specific practice. Consistent practice of movements weakened by spinal cord injury reinforces demand for those functions and encourages adaptive changes in the spinal cord.
In the following section, we’ll discuss the various ways neuroplasticity is involved in the treatment of paraplegia.
Treatment and Management of Paraplegia
Treatment for paraplegia will focus on optimizing the individual’s functional abilities through a variety of interventions. This may involve practicing strengthening exercises or learning alternative methods to perform everyday tasks. By learning how to adapt, individuals can significantly improve their quality of life.
Below, we’ll discuss various interventions that may be involved in the rehabilitation process.
Physical Therapy
Physical therapy for paraplegia focuses on helping individuals strengthen weak muscles, improve their flexibility, and gain/maintain full range of motion through targeted exercises. A physical therapist will create a custom exercise regimen for each client to ensure that their specific rehabilitation goals are met.
Physical therapy can be especially helpful for individuals with incomplete spinal cord injuries because it helps target weakened muscles and strengthen them. This specific and repetitive stimulation helps promote neuroadaptive changes in the central nervous system.
To maximize the outcomes of physical therapy, individuals with paraplegia must make sure to also practice the leg exercises at home. The more you practice, the better the central nervous system gets at recognizing demand for those functions and rewires itself. Utilizing neurorehabilitation devices like FitMi can help engage and motivate users to perform the repetitions they need to promote neuroplasticity and improve their mobility.
Occupational Therapy
Occupational therapy for paraplegia helps individuals develop their functional independence. This primarily involves practicing activities of daily living such as grooming, eating, and dressing, and working on recovering functions and skills related to these tasks.
Individuals with paraplegia typically have great potential to restore their independence because they can use their hands and arms to compensate for limited lower body functions. For example, their ability to grab objects or propel a manual wheelchair is unaffected. As a result, they are often able to move from one location to another and perform many daily activities on their own.
An occupational therapist can help guide individuals through alternative ways to perform activities of daily living to help individuals with paraplegia optimize their independence. For example, they can teach them how to use adaptive tools such as transfer benches to safely get in and out of the shower.
Occupational therapists may also educate individuals on safety measures related to paraplegia and potential sensation deficits, including the importance of daily skin integrity checks to prevent the development of pressure sores.
Orthotic Devices
Orthotic devices like braces and AFOs can help promote correct musculoskeletal alignment in individuals who experience muscle tightness or weakness in their legs. They help hold the affected limb in place to prevent further contractions and mildly stretch tight muscles, or stabilize and support weakened areas.
Pharmaceutical Interventions
Individuals with paraplegia that experience muscle tightness in their legs may also benefit from pharmaceutical interventions like Botox injections or muscle relaxants.
These will help prevent involuntary muscle contractions and allow individuals to practice exercises without the influence of spasticity.
Understanding Paraplegia: Key Points
Paraplegia refers to paralysis of the lower body that is primarily associated with damage to the spinal cord. Depending on the severity of the damage, individuals can experience varying severities of paralysis throughout their legs which can affect their balance, mobility, and functional independence.
Fortunately, individuals typically have unaffected control of their arms and should be able to learn effective ways to compensate for limited leg functions. Additionally, some individuals may be able to recover motor control in their legs through intensive, task-specific training.
We hope this article helped you understand what paraplegia is, how it may affect your everyday life, and how to manage it.