Brain injury survivors who experience foot drop after TBI have difficulties with lifting the front portion of their foot. This may cause the toes to drag when walking, increasing the risk of falls.
While foot drop can be associated with multiple conditions, foot drop after TBI is usually caused by a disruption in communication between the areas of the brain responsible for movement and the muscles involved in ankle mobility. When the brain cannot send the appropriate signals to the muscles to lift the foot, foot drop may occur.
Individuals with foot drop often experience difficulty walking and safely navigating daily activities. Fortunately, there are various treatment options available to help improve foot drop after TBI. Use the links below to jump directly to any section of this article to learn more.
- Causes
- Signs of foot drop
- Impact on daily activities
- Engaging neuroplasticity for recovery
- Treatments
Causes of Foot Drop After TBI
The motion of ankle dorsiflexion involves lifting the front portion of the foot upwards toward the shin. When an injury affects the ability to perform this motion, individuals may be diagnosed with foot drop. While the most common cause of foot drop is nerve injuries, it can also be a symptom of underlying muscular or neurological conditions, such as a traumatic brain injury.
In order to perform voluntary movements, a signal must be transmitted from the brain through the spinal cord and peripheral nerves to the targeted muscles. Disrupting this signal at any point may result in impaired movement. For example, foot drop most often occurs when a peripheral nerve injury in the leg disrupts communication between the brain and the leg muscles.
However, an injury to areas of the brain associated with ankle movement, such as the primary motor cortex, can also result in foot drop. Without the appropriate signals coming from the brain, the muscles associated with lifting the foot are not told when to contract. Furthermore, because the brain can’t tell these muscles to counteract the force of gravity pulling downward on the toes, foot drop occurs.
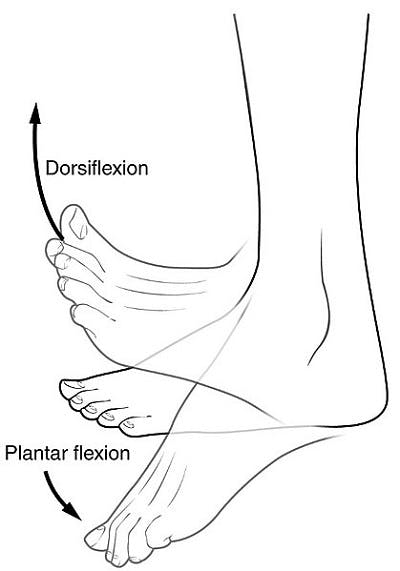
Image Credit: Wikipedia
Although foot drop is usually a direct result of a disruption in the brain’s signals to the targeted muscles, it can also be caused by muscle weakness. Because the causes of foot drop may vary, it’s important to consult with one’s doctor and obtain an accurate diagnosis.
Signs of Foot Drop After TBI
One of the most common signs of foot drop after a brain injury is ankle weakness. However, there are other symptoms that doctors or therapists may look for in order to make an accurate diagnosis.
Signs of foot drop after TBI can include:
- Toes curling toward the balls of the feet
- Persistent corns on the base of the foot
- Frequent stumbling and/or falls
- Changes in gait (manner of walking)
It is also common for individuals with foot drop to experience numbness or tingling in the top of the foot. This is especially common among those with a nerve injury or underlying neurological condition.
Impact of Foot Drop on Daily Activities
Difficulties with ankle dorsiflexion due to foot drop can impact participation in many activities, such as putting on shoes, getting into and out of the shower, and tapping the foot to music. However, the inability to perform ankle dorsiflexion is usually most evident when walking.
In order to walk safely and effectively, the heel usually hits the ground before the toes when stepping forward. If the toes are unable to be raised, they either drag when stepping or hit the ground first.
To combat this, individuals may change their gait pattern (how they walk). Many develop a steppage gait, where they raise the leg up higher at the hip and knee to keep the toes from dragging. This may almost make them look like they are climbing stairs rather than walking on a flat surface. A steppage gait requires more energy and may cause further injuries due to safety concerns and overexertion of the hip and back muscles.
Individuals should consult their doctor if they experience any new or recurring symptoms that may be related to foot drop. That way, they can more accurately determine the cause and administer the appropriate treatment.
Importance of Neuroplasticity for Recovery
Since foot drop after TBI often occurs as a result of impaired communication between the brain and the muscles involved in lifting the foot, restoring this communication pathway is essential for recovery. Fortunately, the brain has the natural ability to rewire itself by strengthening existing neural connections and creating new ones through a process known as neuroplasticity.
As neural connections are restored, the brain may be able to accurately send nerve signals to the affected muscles, improving mobility and overall function. To activate neuroplasticity, it is vital to consistently and repetitively practice targeted exercises involving lost functions. The more a movement is practiced, the more the brain will reinforce and strengthen the neural connections required for that function.
Treating Foot Drop After TBI
Foot drop treatments that optimize neuroplasticity can be some of the most effective options. While a few common treatments for foot drop are listed below, it’s important for individuals to consult with their doctor and/or therapist for personalized recommendations.
Effective treatments for foot drop after TBI may include:
Foot Drop Exercises
To restore communication between the brain and the muscles of the leg, it is essential to rewire the brain through neuroplasticity to control dorsiflexion once again. The best way to achieve this is through frequently practicing targeted exercises, usually with the guidance of a physical therapist.
Even minimal movement is beneficial and can help stimulate recovery. In fact, individuals who are unable to actively dorsiflex their ankle at all can improve foot drop by supporting their foot through correct movement patterns.
Recommended foot drop exercises may include:
- Passive ankle dorsiflexion: To complete this passive exercise, sit in a comfortable position and cross one leg over the other, so that the affected foot is easy to reach. Then, use the hands to bend the foot up towards the knee and back down.
- Assisted toe raises: In a seated position, place the front portion of the non-affected foot underneath the affected one. Then, use the stronger foot to lift the front portion of the affected foot, making sure to always keep both heels on the ground. Hold for a few seconds, then slowly lower the foot back down.
- Negative toe raises: After regaining some movement in the foot, start this exercise by pointing the toes up toward the body as much as possible. Then, instead of quickly letting the foot fall down, slowly lower the foot back to a neutral position.
- Ball lifts: Sit with both feet flat on the floor. Place a tennis ball on the floor and hold it between the feet. Then, using both feet, bend at the ankle to slowly raise and lower the ball.
As mobility improves, strengthening exercises using resistance bands can also be added. In addition to boosting recovery, keeping the foot and ankle moving is essential for improving blood flow, lowering the risk of contractures, and reducing the risk of learned non-use.
Functional Electrical Stimulation
While therapeutic exercises are usually the best way to promote neuroplasticity and improve foot drop after TBI, some survivors may benefit from additional treatments, such as functional electrical stimulation (FES). By sending small electrical impulses into the affected muscles of the leg, FES can create a muscle contraction similar to what would occur if the brain itself was telling the muscle to engage.
Reactivating these muscles through FES encourages mobility and engages neuroplasticity. Ideally, FES should be used in conjunction with therapeutic exercises to maximize the chances of recovery.
Ankle-Foot Orthotics (AFOs)
Because foot drop makes it difficult to move and walk safely, therapists often recommend using an ankle-foot orthotic, or AFO brace. AFOs provide support for the foot and ankle to prevent the toes from scuffing the floor when walking, lowering the risk of falls.
There are many types of AFOs available, including the Flex AFO recently developed by Flint Rehab. A physical therapist can be a great resource to help survivors determine which AFO brace is most suitable for their needs.
While AFOs can be helpful, they do not encourage recovery through neuroplasticity like the other treatments listed above. AFOs are considered compensatory tactics, which help to make up for lost functions without necessarily trying to improve those functions. Therefore, while AFOs can help individuals walk more safely and effectively, they are not good long-term replacements for those hoping to improve their ankle mobility.
This is because always using compensatory tactics, such as an AFO brace, can lead to learned non-use. When the muscles involved in lifting the foot are consistently unused due to being stabilized by an AFO brace, any remaining function in those muscles gradually deteriorates until the body has learned not to use those muscles at all.
To combat this, it is essential to take breaks from using the AFO and practice foot drop exercises. This will help stimulate the brain and activate neuroplasticity to promote recovery.
Surgery
Severe cases of foot drop may require surgical interventions. Different surgical treatments, such as nerve transfers and decompressive surgeries, can help improve dorsiflexion.
Nerve transfers involve taking “donor nerves” from other parts of the body and using them to connect the ends of the divided or damaged nerves. Decompressive surgery is a procedure that helps relieve pressure on the nerves, which can also help improve dorsiflexion.
These surgeries are generally most effective if there is an injury to the peripheral nerves in conjunction with a TBI, as may occur when the leg has also sustained trauma at the time of one’s injury. Because surgical interventions are highly invasive, they should only be considered when all other treatment options have been exhausted.
Recovering from Foot Drop After TBI
Foot drop after TBI can make it difficult to walk and safely navigate daily activities. The inability to lift the front portion of the foot (dorsiflexion) is caused by the disruption of signals between the brain and muscles.
The best way to recover from foot drop is to activate neuroplasticity and restore neural connections. This can be achieved by the consistent and repetitive practice of targeted exercises, both active and passive.
Still, many survivors benefit from using multiple treatment options, including AFO braces, electrical stimulation, and a variety of exercises. Therefore, it’s important for individuals to consult with their doctor to obtain an accurate diagnosis and rehabilitation plan.