Complications of paraplegia can arise immediately after spinal cord injury, years later, or anytime in between.
Therefore, it’s essential to be aware of complications and understand what you can do to prevent them from worsening.
This article will go over 9 common complications of paraplegia and how to manage them.
Complications of Paraplegia
The development of secondary complications after spinal cord injury can significantly affect rehabilitation outcomes and quality of life. Complications of paraplegia can affect energy levels, quality of sleep, mood, and motivation for recovery.
By minimizing the onset of complications through preventive measures, individuals can improve their recovery outcomes. Additionally, even if your spinal cord injury occurred years ago, you can still work on recovery. It’s never too late!
You’re about to learn about 9 common complications of paraplegia:
1. Spasticity

Spasticity refers to involuntary muscle contractions in areas below your level of injury. It occurs because SCI disrupts the communication between your brain and body.
As a result, your muscles become hypersensitive to stimuli. Additionally, because they do not receive signals from the brain to relax, they remain contracted for extended periods.
Poorly managed spasticity can lead to other complications of paraplegia such as contractures, pain, poor quality sleep, and difficulty with transferring or walking.
However, moderate spasticity can also be beneficial. For example, individuals with paraplegia can take advantage of increased tone in their leg to prop themselves up when performing transfers and standing.
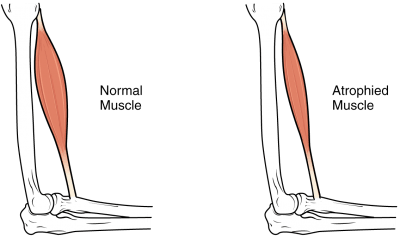
2. Muscle Atrophy
One of the most common complications of paraplegia is muscle atrophy due to reduced physical activity.
Muscle atrophy is when your muscles shrink from disuse. Think ‘use it or lose it.’ Our bodies are constantly adapting based on our everyday actions and when you significantly reduce movement and weight-bearing in the legs, the muscles will shrink to preserve energy.
Low muscle mass can increase your risk of injury, cause blood to pool in your legs, and slow down your metabolic rate. Even if you have severe paraplegia, passive movement of your legs is essential to promote circulation, metabolism, and stimulate the spinal cord.
3. Bowel and Bladder Dysfunction

Another common complication of paraplegia is bowel and bladder dysfunction. After spinal cord injury, patients may be unable to feel when their bladders are full or when they need to empty their bowels.
Additionally, they may not be able to control the contracting or relaxing of their urethral or anal sphincters, so accidents or physical discomfort can occur.
4. Autonomic Dysreflexia

Autonomic dysreflexia is a complication that can occur in individuals with T6 level spinal cord injuries and above. It describes the body’s hyperactive response to sensory stimuli due to disrupted communication between the brain and body.
The autonomic nervous system is responsible for involuntary body functions like temperature regulation, heart rate, and blood pressure. As a result, when areas below the level of injury are stimulated, individuals may experience:
- A sudden rise in resting blood pressure
- Anxiety
- Headaches
- Blurry vision
- Sweating
- Blotchy skin
Autonomic dysreflexia can be caused by extreme temperatures, skin irritations, tight clothes, and a full bladder. Therefore, it’s essential to be aware of your surroundings and avoid sitting or lying on something that can irritate the skin.
5. Pressure Sores
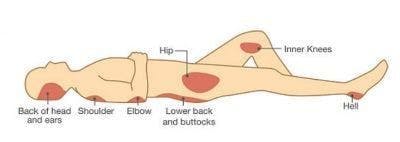
Individuals with paraplegia have an increased risk of developing pressure sores due to lack of movement.
Typically, people start to feel restless after sitting or lying in the same position for too long and will move around. However, due to loss of sensation following a spinal cord injury, many paraplegics may not feel the urge to move around.
Pressure sores are the result of prolonged pressure on the skin. Blood flow is cut off and tissues start to die, which makes the skin more susceptible to breakdown.
Pressure sores typically occur in areas of the body where the bones and skin are very close together like the elbows, shoulders, hips, knees, and ankles.
6. Pain

About 40-60% of all spinal cord injury patients develop neuropathic pain below their level of injury.
This type of pain is caused by damage to the nerves. Some people describe feeling pins and needles while others may feel burning or stabbing sensations.
People with paraplegia can also experience musculoskeletal pain above their level of injury from increased dependence of the arms. For example, you might overexert your arms when moving around in a wheelchair for too long.
Luckily, this type of pain is more bearable and can usually be relieved through rest.
7. Deep Vein Thrombosis
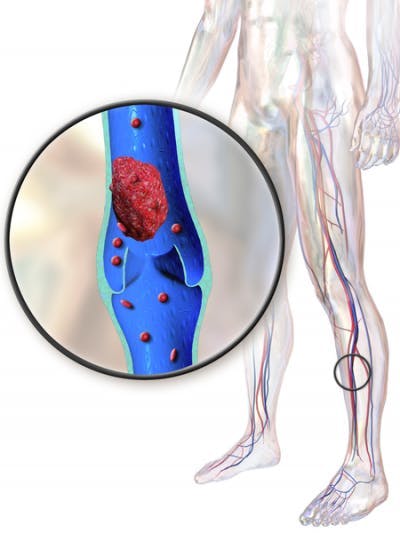
Deep vein thrombosis is a complication of paraplegia that occurs when a blood clot forms in the legs due to lack of movement. It can cause swelling, aching, and poor blood flow in the lower body.
Additionally, if part of the blood clot travels up to the lungs, it can cause a pulmonary embolism. Pulmonary embolisms occur when blood clots block arteries in the lungs, resulting in sudden breathing difficulties and chest pain.
8. Osteoporosis
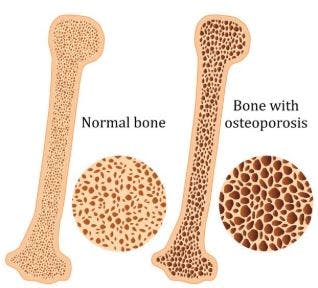
After a spinal cord injury, mobility becomes restricted, so many people can’t walk as much as they used to. Because the bones in the legs no longer bear as much weight, they lose bone mineral density below their level of injury.
Generally, the severity of injury is correlated to the severity of bone loss. Therefore, individuals with complete spinal cord injuries experience more severe osteoporosis than individuals with incomplete spinal cord injuries.
The effects of osteoporosis are most significant in the initial 12-18 months following a spinal cord injury. It’s suggested that on average, SCI patients experience bone loss at a rate of 4% per month.
While unmanaged osteoporosis will continue to progress for several years, it occurs at much a slower rate.
9. Depression or Anxiety

Because spinal cord injuries can require major changes to one’s lifestyle, the development of mental health complications like depression and anxiety extremely common. About 11-37% of SCI survivors experience depression and 15-32% experience anxiety.
Mental health disorders are caused by chemical imbalances in the brain. Both anxiety and depression can significantly affect your quality of life as they interfere with your motivation, energy levels, quality of sleep, and mood.
Now that you understand what these 9 complications of paraplegia are, let’s discuss what you can do to manage them.
Managing Complications of Paraplegia
Everyone experiences complications of paraplegia differently, so it’s essential to take a personalized approach to management. Generally, a combination of various management interventions proves the most effective, so you may need to go through some trial and error to find what works for you.
Below, we’ve listed some interventions that can help you manage complications of paraplegia:
- Participate in physical therapy. Physical therapy can help you maximize your mobility after spinal cord injury through exercise. A trained professional will assess your functional abilities and create a personalized exercise regimen that will help promote circulation, prevent stiffness, and strengthen weakened muscles.
- Increase movement throughout the day. As you’ve just learned, many complications of paraplegia like muscle atrophy, pressure sores, and deep vein thrombosis are caused by reduced mobility. Moving throughout the day (even if you have to use your arms to passively move the legs) is essential for bone health, muscle health, efficient circulation, and optimal functioning of the body. Click here to discover exercises for paraplegics»
- Take medications as necessary. Many complications of paraplegia can be managed through medications. For example, muscle relaxants can help temporarily relieve spasticity, blood thinners can help break up blood clots, laxatives can help promote bowel movements, and antidepressants can help improve mood and energy levels for those with depression.
- Wear comfortable clothes. If you have a T6 or higher-level SCI, avoid wearing tight clothes that can trigger autonomic dysreflexia.
- Be mindful of your surroundings. Being aware of your surroundings and avoiding stimuli that can trigger hyperactive reactions after SCI is essential. Individuals should try to avoid extreme temperatures and sitting or lying on objects that can irritate the skin.
- Follow a schedule. Following a bowel and bladder management schedule can help individuals better predict their bowel movements and avoid accidents. For example, you’ll need to plan when to take medications or when to empty your catheter.
- See a psychotherapist. Psychotherapy can help individuals with paraplegia learn effective ways to cope after spinal cord injury. Living with SCI is just as much a psychological challenge as it is a physical one. Without the right mentality, recovery may be stalled.
- Join a spinal cord injury support group. Surrounding yourself with people that understand what it’s like to live with paraplegia and its complications can be a great way to cope and learn.
- Consider alternative treatments. Alternative treatments like massage therapy and acupuncture are generally more affordable and have less severe side effects than pharmacological treatments.
- Perform daily skin inspections. If you lose sensation in your legs after a spinal cord injury, performing daily skin inspections is essential to identify pressure sores in its early stages and prevent them from worsening.
- Wear orthotic devices. Orthotic devices like braces and splints can help support proper alignment of the bones and muscles, especially if they’re affected by spasticity. Similarly, wearing compression garments can help consistently apply pressure to the skin to promote circulation.
Living with Complications of Paraplegia

By learning how to adapt and manage their complications, individuals with paraplegia can optimize both their physical and mental health.
Generally, those with more severe spinal cord injuries are more susceptible to complications; however, it’s always a good idea to be aware of problems that can arise and prepare for them.
Hopefully, this article helped you better understand the various complications that can result from paraplegia and how to manage them. Good luck!