No products in the cart.
No products in the cart.
No products in the cart.
No products in the cart.
Home » Neurological Recovery Blog » Stroke » Post Stroke Symptoms Getting Worse? How to Get Back on Track
Last updated on February 23, 2023

Are your post stroke symptoms getting worse? Sometimes regression after stroke is a normal part of the recovery process, but it can also be a sign of additional medical complications in some cases. How can you tell if you’re on the right track?
This article will discuss worsening symptoms after a stroke, what a normal regression looks like, and how to continue progressing during your recovery journey. We will also discuss reasons for regression after stroke that may be a cause of concern and warrant further medical treatment.
It is crucial to communicate with your doctor and rehab team if you have concerns about your post stroke symptoms getting worse. They will be able to investigate the cause of your symptom regression and help keep you on the right track to maximize your recovery after stroke.
It’s important to acknowledge that the stroke recovery process does not move in a straight line. Taking two steps forward and one step back is normal. In fact, taking two steps forward and four steps back sometimes is also normal. A good rule of thumb to determine if your regression is normal or not is to take the time to look at the big picture. Is there an overall pattern of progress?
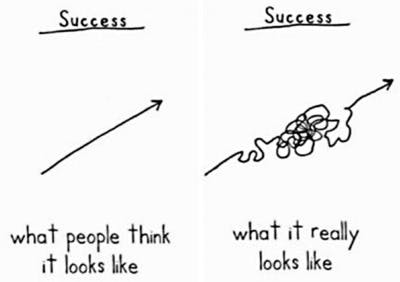
Drawing by Demitri Martin
Stroke recovery is not linear, and most patients experience ups and downs during recovery. However, your backward steps should be overcome by your forward steps in the long run. To track your progress, it’s helpful to keep a journal of your daily activities, improvements, and energy levels. That way, if you experience regression after stroke, you can look to see if any patterns emerge.
For example, you may “regress” on days after rigorous physical therapy and improve the next day. Once you see the pattern, you may not consider it regression. Instead, it’s a sign that you either pushed too hard or that the body is healing. By identifying patterns, you can put your mind at ease whenever it seems like you’re regressing after stroke.
However, if you wake up one morning and the secondary effects of your stroke are dramatically worse than the previous night, then it’s time to seek immediate medical attention. This could be a sign of a medical emergency, which we will discuss later in this article.
The recovery journey is complex and often full of twists and turns. There will be times when it feels you are gaining function quickly and progressing each day. Then there may be periods where you feel your progress has reached a plateau or stalled. This is common for survivors of stroke, however, and is not cause to give up on your rehabilitation goals.
For example, research tells us that the greatest neuroplasticity, or rewiring of neural pathways and connections in the brain, occurs in the first six months after stroke onset. During this time, this heightened state of neuroplasticity, along with spontaneous recovery, allows for quicker improvements in overall function. Consequently, survivors of stroke can become discouraged when progress seems to slow as they move into the next stage of rehabilitation.
If your post stroke symptoms have worsened, take a look at what you have done over the course of the last few days. Changes in routine or activity levels are a common culprit when investigating a regression in function after stroke. Conversely, your body may simply be adapting to your current regimen and need additional stimulation.
To help you pinpoint what may be leading to your seemingly worsening symptoms, here are examples of potential causes of regression after stroke:
Have you started doing anything dramatically different lately? For example, have you started walking a lot whereas you were sedentary before? Conversely, have you been sitting more frequently when you were previously more active?
Big changes to your daily routine can affect your body in a big way, and not always for the better. An example of this is changing your schedule and exercising in the afternoon instead of the morning. If you begin to notice you are too tired to complete all your exercises after this kind of schedule change, this could be contributing to your worsening symptoms.
Whether you changed your activity level or your daily schedule, these changes can have an impact on your progress. If you do make larger changes to your routine, document this along with your progress so you can detect a correlation between the two.
Sometimes new medication can cause negative side effects. For example, some stroke survivors report regression after taking anti-depressants, and they also report the regression reversing itself once they stop taking it.
However, there is a reason these medications were prescribed to you to decrease stroke-related complications. Additionally, some medications are used to manage stroke risk factors, which help prevent another stroke.
Do not tinker with your medication without consulting a doctor. If you suspect a new medication is linked to sudden regression, be sure to talk to your doctor about your concerns before changing your dosage. Instead of weaning off a medication, your doctor may be able to change your prescription to something different to see if your regression improves.

Following a stroke, it is essential to commit yourself to a dedicated rehabilitation plan and perform high repetition of therapeutic exercise to promote the return of your physical function. However, there is such a thing as overtraining and this can contribute to regression after stroke.
Laborious physical activity on one day could manifest in extreme tiredness the next day. This should not be considered a regression. Rather, it’s a sign that the body has been taxed and needs time to recuperate.
If you continue to experience this after each session and begin to note a decline in progress or functional abilities, however, this can be a sign of overtraining. This is why it is important to work closely with your therapy team to progress exercise at a steady, safe rate.
If you are experiencing an acute regression or increased fatigue after exercise, try to scale back the intensity of your exercise slightly and see if that helps. Be mindful that the brain takes up more energy as it is healing, which we will discuss next.
Post-stroke fatigue is a common secondary effect of stroke and can play a major role in recovery, contributing to symptoms that seem to be worsening. This fatigue can include a decrease in both mental and physical energy levels, affecting the ability of a survivor to participate in daily or rehab activities.
Following stroke, movement will likely involve greater energy requirements, especially if stroke symptoms include hemiparesis or hemiplegia (weakness or paralysis of one side of the body). Due to this, daily tasks that were once simple or second nature may now be exhausting and take an increased amount of time and energy.
Furthermore, stroke can lead to sleep disturbances and have a negative effect on progress as our bodies require adequate sleep to fully recover. Excessive sleepiness after stroke could be normal, or it could be a sign of other medical complications like sleep apnea. Talk to your doctor if you are experiencing excessive sleepiness or other sleep-related changes after stroke.
Changing emotions after stroke are not necessarily a sign of regression. It’s normal for stroke patients to experience grief or anger, which usually pass with time. However, extreme emotional swings could be a sign of pseudobulbar affect, which should be discussed with your doctor.
Additionally, post-stroke depression is a secondary effect that impacts anywhere between 18-33% of stroke survivors. This can contribute to decreased motivation to participate in rehabilitation as well as increased fatigue. Depression should be taken seriously and there are treatments available to help combat this. Talk with your doctor if you think you are experiencing signs and symptoms of depression.
Sometimes stroke patients get worse once they stop participating in rehabilitation and stop exercising. Research supports that adherence to a rehabilitation plan leads to greater functional outcomes for stroke survivors. Discontinuing rehabilitation can lead to deterioration of functional abilities and worsening symptoms after stroke.
If you are having difficulty finding motivation to perform your exercises, try switching up your program to incorporate interactive activities or hobbies. Your physical or occupational therapist is a great resource for this and can help you find therapeutic activities that are beneficial and motivating for you.
If you can’t identify the cause of your regression, try talking with your physiatrist, neurologist, or therapist about your concerns. They may be able to help identify potential causes of regression after stroke and provide helpful insight or techniques to boost your progress.
Post stroke regression is a mysterious phenomenon and doctors are often unable to pinpoint exactly what’s causing the regression. A change in progress might be chalked up to “every stroke is different, so every recovery is different.”
However, you know your body best and it is okay to bring up your concerns and to seek a second medical opinion if needed. Throughout this process, continue to meticulously track your progress so that you have something to reference.
If you think you’re going through the normal ebb and flow of recovery (i.e. a small regression), here are 4 ways to work through it and get your results flowing again.
Stroke recovery is not a race. Although a speedy recovery is what everyone wants, it’s easy to burn yourself out by trying to do too many things at once. The fastest gains in function may occur in the first 6 months after stroke onset, but the recovery process will continue for years after stroke.
During stroke recovery, your brain is rapidly trying to heal itself, which uses up a lot of your mental and physical stamina. When you push yourself too hard, you can increase levels of fatigue and prevent your brain and body from recovering fully between sessions. To avoid regression, it’s best to aim for a slow and steady pace instead of rushing and eventually experiencing burnout.
Sleep is incredibly important during stroke recovery as it gives your brain a chance to rest and recharge, facilitating neuroplasticity. If you don’t sleep when your body wants and needs to, this can slow your recovery. Your brain needs a chance to heal and recharge, so practice good sleep habits and make rest a priority.
Also, it’s important to know that the desire for lots of sleep after stroke is not a sign of regression. Increased sleep requirements are perfectly normal and healthy for a stroke survivor.
Consistency is key when it comes to stroke recovery. If you work on your rehabilitation just a little bit each day, you will see big results over the long run. If you become inconsistent, however, you put yourself at risk of backsliding and regression.
Not only may skipping your home exercises result in regression, but overdoing them may also hinder your progress. Consistent stimulation with gradual progression is the best way to rewire your brain. Without consistency, the new connections in your brain can start to weaken and you might lose progress.
Aside from consistency, the best way to rewire your brain and heal after stroke is high repetition of therapeutic exercises. When you repeat something, you activate neuroplasticity and strengthen the connections in your brain that control that task.
For example, the more you practice your hand therapy exercises, the stronger the connections in your brain that control hand function will become. Therefore, if you find yourself regressing in a particular area of your recovery, start utilizing repetitive practice to get yourself back on track.
Overall, it’s important to understand that stroke recovery naturally has an ebb and flow, and small changes are often part of the normal recovery journey. However, if you experience rapid, sudden worsening of stroke secondary effects without explanation, seek medical attention immediately.
Stroke risk is greater for individuals who have already experienced one stroke, so it is important to monitor for stroke warning signs. This can include drooping of the face, weakness of one arm or side of the body, slurred speech, and sometimes headache or vision changes. If you notice any new or worsening stroke symptoms, call 911 immediately. Timely medical treatment is crucial to reduce the secondary effects of stroke and potentially save a life.
Additional causes of regression after stroke that warrant medical attention include:
These conditions can all lead to more sudden regression after stroke and require medical attention. If you are concerned about your worsening symptoms, contact your doctor and discuss the changes you’ve noticed.
The stroke recovery process is long and can come with many challenges, including the feeling that symptoms are getting worse instead of better. However, know that regression after stroke is common and often temporary. This can be impacted by factors such as new medications, schedule changes, or excess fatigue. As you continue to stay consistent with your rehabilitation, you will be able to move forward past these plateaus in progress.
Understanding regression after stroke involves carefully interpreting the difference between big declines that deserve medical attention and small declines that are normal. Continue to track your progress and symptoms and keep your doctor informed of what’s happening. If you notice a rapid decline or the presence of stroke symptoms such as increased weakness, impaired speech, drooping of the face, or confusion, seek immediate medical treatment.
Overall, when you zoom out and look at the big picture, there should be a pattern of growth. Little setbacks are normal and expected, so continue to work towards recovery and celebrate small victories. Your rehab team is an excellent resource if you are experiencing regression after stroke, and consistency is the key to forward progress.
Get our free stroke recovery ebook by signing up below! It contains 15 tips every stroke survivor and caregiver must know. You’ll also receive our weekly Monday newsletter that contains 5 articles on stroke recovery. We will never sell your email address, and we never spam. That we promise.


Do you have these 25 pages of rehab exercises?
Get a free copy of our ebook Full Body Exercises for Stroke Patients. Click here to get instant access.
“My name is Monica Davis but the person who is using the FitMi is my husband, Jerry. I first came across FitMi on Facebook. I pondered it for nearly a year. In that time, he had PT, OT and Speech therapy, as well as vision therapy.
I got a little more serious about ordering the FitMi when that all ended 7 months after his stroke. I wish I hadn’t waited to order it. He enjoys it and it is quite a workout!
He loves it when he levels up and gets WOO HOOs! It is a wonderful product! His stroke has affected his left side. Quick medical attention, therapy and FitMi have helped him tremendously!”
FitMi is like your own personal therapist encouraging you to accomplish the high repetition of exercise needed to improve.
When you beat your high score or unlock a new exercise, FitMi provides a little “woo hoo!” as auditory feedback. It’s oddly satisfying and helps motivate you to keep up the great work.
In Jerry’s photo below, you can see him with the FitMi pucks below his feet for one of the leg exercises:
Many therapists recommend using FitMi at home between outpatient therapy visits and they are amazed by how much faster patients improve when using it.
It’s no surprise why over 14,000 OTs voted for FitMi as “Best of Show” at the annual AOTA conference; and why the #1 rehabilitation hospital in America, Shirley Ryan Ability Lab, uses FitMi with their patients.
This award-winning home therapy device is the perfect way to continue recovery from home. Read more stories and reviews by clicking the button below:
Grab a free rehab exercise ebook!
Sign up to receive a free PDF ebook with recovery exercises for stroke, traumatic brain injury, or spinal cord injury below: