Traumatic brain injury involuntary movements occur when the communication between the brain and the muscles is disrupted. There are various types of post traumatic movement disorders that can develop depending on the area and severity of the injury, such as tremors, dystonia, or tics.
This article will discuss the causes of TBI involuntary movements, the different types, and how to find the best treatment.
Use the links below to jump straight to any section:
- How a TBI Causes Involuntary Movements
- Types of Involuntary Movement Disorders
- Delayed Onset of TBI Symptoms
- Restoring Movement with Neuroplasticity
- Treatment for Involuntary Movement Disorders
Causes of Traumatic Brain Injury Involuntary Movements
A traumatic brain injury can disrupt communication between the brain and the body. Without proper communication, the muscles are unable to receive signals from the brain, and the brain may not receive feedback from the muscles. This can result in impaired motor control. Studies have shown that involuntary movement disorders have been reported in about 22.6% of survivors with a severe head injury, with 12.2% of individuals reporting persistent symptoms.
Of note, persistent post traumatic movement disorders are rarely experienced by survivors with a mild or moderate traumatic brain injury, and only 5.4% of severe brain injury survivors report significant disability due to involuntary movement disorders.
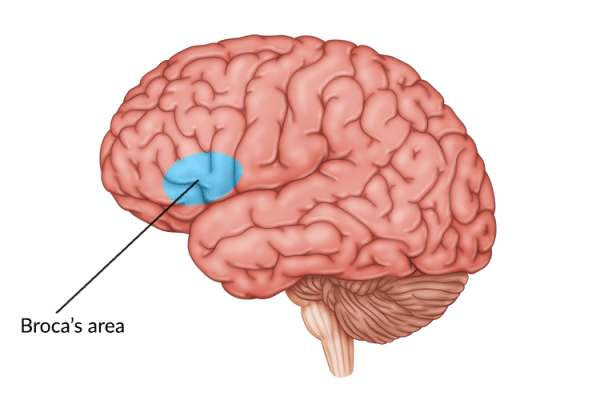
The type of involuntary movement disorder that develops depends on which area of the brain is injured. For example, common causes of post traumatic movement disorders include:
- Primary motor cortex damage: can cause muscle weakness or paralysis
- Cerebellum damage: can cause tremors and/or loss of balance and coordination
- Basal ganglia damage: can cause uncontrollable twitching, spasms, or dystonia
- Thalamus damage: can cause apraxia (difficulties with motor planning) or other motor impairments
Since post traumatic movement disorders may have an immediate or delayed onset, studies report a wide range of prevalence, with anywhere between 13-66% of TBI survivors experiencing movement disorders.
Fortunately, many involuntary movements caused by TBI damage can be managed through rehabilitative techniques.
Types of Involuntary Movement Disorders After TBI
Understanding the various types of traumatic brain injury involuntary movements that can occur is important in order to receive the appropriate treatment and promote recovery.
Some of the most common types of movement disorders after TBI include:
1. Tremors
What it looks like: unprovoked, uncontrollable, rhythmic shaking
Tremors are one the most common types of involuntary movements that occur after a brain injury. Studies show that about 9% of severe TBI survivors experience persistent tremors, while nearly half of all children with traumatic brain injuries experience tremors, lasting up to 18 months. These tremors are characterized by an uncontrollable, rhythmic shaking of different parts of the body, typically the hands.
Tremors are further classified into different categories, including:
- Resting tremors: occur when the muscles are relaxed, such as when the hands are resting in an individual’s lap.
- Action tremors: occur when the muscles are in use. There are many types of action tremors, including postural tremors (occur when an individual holds a position against gravity) and intention tremors (occur when completing a purposeful movement).
The most frequent types of tremors that develop after a head injury are cerebellar tremors, which as the name implies, are caused by damage to the cerebellum. They are a type of action tremor that only occurs at the end of a movement.
2. Dystonia
What it looks like: slow, repetitive twisting movements
Dystonia is another common involuntary movement disorder that occurs from damage to the basal ganglia. Dystonia refers to slow, repetitive twisting movements. These involuntary muscle contractions often force people into abnormal positions. About 4% of severe TBI survivors experience dystonia after brain injury.
This can include different types of dystonia such as:
- Focal dystonia: affects only part of the body such as the eyes, jaw, mouth, neck, arms, or legs. A more specific type of focal dystonia is known as cervical dystonia, which causes spasms in the neck.
- Segmental dystonia: affects two or more adjacent muscle groups simultaneously. For example, survivors may experience spasms in the jaw and neck at the same time.
- General dystonia: affects the whole body.
Generally speaking, movements resulting from dystonia occur on the opposite side of your body from where the injury occurred. For instance, if you experience a left-hemisphere brain injury, it is likely you will experience dystonia on the right side of the body. Though less common, dystonia may also cause the torso to bend or writhe.
3. Chorea
What it looks like: provoked, uncontrollable, rhythmic, dance-like movements
The word chorea comes from a Greek term meaning “to dance”. This is due to characteristic brief, repetitive movements of chorea, which tend to start in one body part and move abruptly to another part. Chorea is caused by damage to the basal ganglia.
Hemiballismus is a severe secondary type of chorea, which involves an aggressive, involuntary flinging of the arm and/or leg on one side of the body. Those with hemiballismus usually exhibit wider and more vigorous movements than those with primary chorea due to extended damage in the thalamus. Chorea can often occur simultaneously with another movement disorder known as athetosis.
4. Athetosis
What it looks like: slow, flowing, writhing movements
Athetosis refers to a stream of slow, flowing, writhing movements. This involuntary movement disorder primarily occurs in the hands, feet, and torso. Both chorea and athetosis are caused by overactivity in the basal ganglia, usually due to excess dopamine in the brain.
5. Clonus
What it looks like: rhythmic shaking after a muscle is stretched
Clonus refers to a hyperactive stretch reflex that is often mistaken for a tremor because the symptoms are similar. Both conditions can cause rhythmic shaking that is painless, and mainly occur in the arms or legs. However, a distinct feature of clonus is that it is triggered and/or exacerbated by stretching the affected limb.
Similar to other movement disorders however, clonus often occurs when the electrical signals sent by the brain to the muscles are disrupted. Without proper stimulation from the brain, the muscles do not know whether to contract or relax. This uncertainty causes the muscles to do both.
6. Myoclonus
What it looks like: unprovoked, unrhythmic muscle spasms
Though myoclonus sounds similar to clonus, it is a distinct disorder that does not cause rhythmic shaking nor does it change in response to stretching. Myoclonus refers to sudden muscle spasms that can happen at rest or during active movement.
Many individuals experience myoclonus throughout their life such as when they hiccup or jerk awake just before falling asleep. However, myoclonus after a head injury tends to be more severe and frequent. While it may affect the limbs, it may also affect the palate or the oculomotor (eye movement) muscles.
7. Parkinsonism
What it looks like: a combination of involuntary movement disorders
Parkinsonism is an umbrella term that refers to a group of movement disorders that share similar symptoms. It typically occurs after repeated head trauma.
Symptoms of Parkinsonism can include:
- Resting tremor
- Stiff muscles
- Slow movements
- Shuffling gait
- Difficulty with balance and/or walking
Parkinson’s Disease is the most common type of parkinsonism that occurs. However, there are several other types including drug-induced parkinsonism, vascular parkinsonism, and post-traumatic parkinsonism (caused by damage to the cerebellum or basal ganglia). Approximately 3.1% of individuals with TBI experience post-traumatic parkinsonism, and that percentage increases to 11.6% in those with TBI after age 65. Post-traumatic parkinsonism often has a delayed onset, with an average estimated onset of 3.3 years after TBI.
Parkinsonism can also cause uncontrolled, repetitive movements known as tics (see below).
8. Tics
What it looks like: sudden, repetitive movements or vocalizations
Tics are primarily involuntary movements that occur from damage to the basal ganglia, poor communication between different brain structures, or excess dopamine in the brain. Tics can cause individuals to make sudden, repetitive movements. Though most tics develop within the first few weeks after a brain injury, some may appear up to one year post-injury.
9. Gait Apraxia
What it looks like: uncoordinated movements while walking
Apraxia is a condition that causes difficulty with planning, coordinating and executing voluntary movements. There are different types of apraxia that can manifest, depending on the areas of the brain affected. For instance, damage to the cerebellum or frontal lobe can result in gait apraxia, which refers to the loss of ability to properly use the lower limbs. This can cause difficulty walking and/or maintaining balance.
10. Other Movement-Related Disorders
In addition to causing involuntary movements, a brain injury can also cause a variety of coordination disorders. These are typically caused by damage to the cerebellum, and can affect the ability to precisely perform voluntary movements. Many of these disorders can make it difficult to control the arms, legs, or trunk.
Movement-related disorders that may occur after a brain injury can include:
- Ataxia: is a coordination disorder that can make it difficult to perform everyday movements such as reaching for an object or walking. It often involves damage to the cerebellum, and may occur even following mild TBI. Individuals with ataxia of the legs are more prone to falls and may take wide, staggering steps when walking.
- Dysmetria: is when an individual cannot judge how far and how quickly their arms need to move to carry out a smooth purposeful movement. For instance, when reaching for an object, they will usually miss the mark.
- Apraxia of Speech: is a condition in which individuals cannot coordinate the muscles used for speech. As a result, they may make irregular mouth movements and have trouble speaking.
- Nystagmus: is a condition that makes it difficult to coordinate eye movements. This can cause the eyes to seem like they are bouncing around.
These types of movement and coordination disorders can often prevent individuals from controlling their arms, legs, or trunk. They may even inhibit them from using the muscles of their mouth or eyes accurately. Therefore, obtaining proper treatment is essential in order to improve muscle coordination after head injury.
Consult with your doctor or therapist if you notice any new or recurrent symptoms from any of the involuntary movement disorders listed above. With a proper diagnosis, treatment can be administered and rehabilitation started.
Delayed Onset of Involuntary Movements After TBI
Many involuntary movement disorders are not apparent right after the injury. Some individuals may experience a delayed onset of TBI symptoms or secondary effects. One study roughly estimated 57% of individuals reported new symptoms within one year of initial injury. This included a combination of different symptoms including physical, emotional, and cognitive effects.
Therefore, it’s important to keep track of any new recurrent symptoms and seek proper medical care. This can help lower the chances of TBI symptoms worsening over time or experiencing a decline during your recovery.
Speak to your doctor if you have any questions or concerns about your symptoms.
How Neuroplasticity Can Help Improve Traumatic Brain Injury Involuntary Movements
To treat TBI involuntary movements, the communication between the brain and the rest of the body must be restored. This can be accomplished with the help of neuroplasticity, the brain’s ability to heal and rewire itself.
After a brain injury, many of the neural pathways used for communication between the brain and body may become damaged or destroyed. However, neuroplasticity can help strengthen existing neural pathways and create new ones, allowing the brain to adapt and recover from injury.
The best way to stimulate the brain and activate neuroplasticity is through repetitive exercise, also known as massed practice. Stimulating the brain after a head injury can help reduce the symptoms of post-traumatic involuntary movement disorders.
Practicing a movement consistently will help the brain create new neural pathways for those specific movements. With time, pathways associated with targeted movements may be rewired and reinforced in healthy, undamaged regions of the brain.
The stronger neural pathways, the better communication between the brain and body. And with better communication, the higher the chances of restoring motor control.
Treatment for Traumatic Brain Injury Involuntary Movements
Every brain injury is different, and treatment for involuntary movements may vary depending on the type and severity of the disorder. If your post-traumatic movement disorder is severe or causing you pain, doctors may prescribe medication such as baclofen. This helps relax the muscles and prevent spasms.
However, medication is often only a temporary solution because it does not address the root cause of a post-traumatic movement disorder, which is the lack of communication between the brain and muscles.
As previously mentioned, to improve the neural connections needed to regain functions, neuroplasticity must be activated through massed practice. Therefore, it is crucial to attend physical, speech, and/or occupational therapy sessions and practice rehabilitation exercises to promote recovery.
Each of these therapies utilize unique techniques and yield unique benefits for improving motor control, including:
- Physical Therapy: focuses on improving mobility, coordination, and strength. Physical therapists may use personalized stretches, hands-on techniques, repetitive exercises, and modalities to improve affected movements.
- Speech Therapy: assesses and treats oral motor concerns including dysphagia (difficulty swallowing) and speech difficulties through practicing specialized exercises.
- Occupational Therapy: addresses difficulty participating in daily tasks due to involuntary movements. To improve independence, occupational therapists may use activity-based exercises and/or introduce compensatory techniques and adaptive equipment.
- Home Exercise Programs: rehabilitative therapists usually recommend participating in a home exercise program to maximize the chances of recovery. They may provide a written exercise program or suggest usinghome therapy devices such as FitMi, aninteractive therapy device designed to improve full-body mobility.
Depending on what types of involuntary movements you are experiencing, you may participate in more than one type of rehabilitative therapy. Starting therapy promptly can improve recovery, so be sure to start as soon as possible after symptoms appear.
Understanding Involuntary Movements Post-TBI
Traumatic brain injury involuntary movements can make it difficult to perform daily activities and continue with everyday life. Fortunately, the brain is capable of utilizing neuroplasticity to improve motor control. The most effective way to promote neuroplasticity is through high repetition of exercises.
We hope this article helped you understand the most common types of TBI involuntary movements, and the best ways to promote recovery.